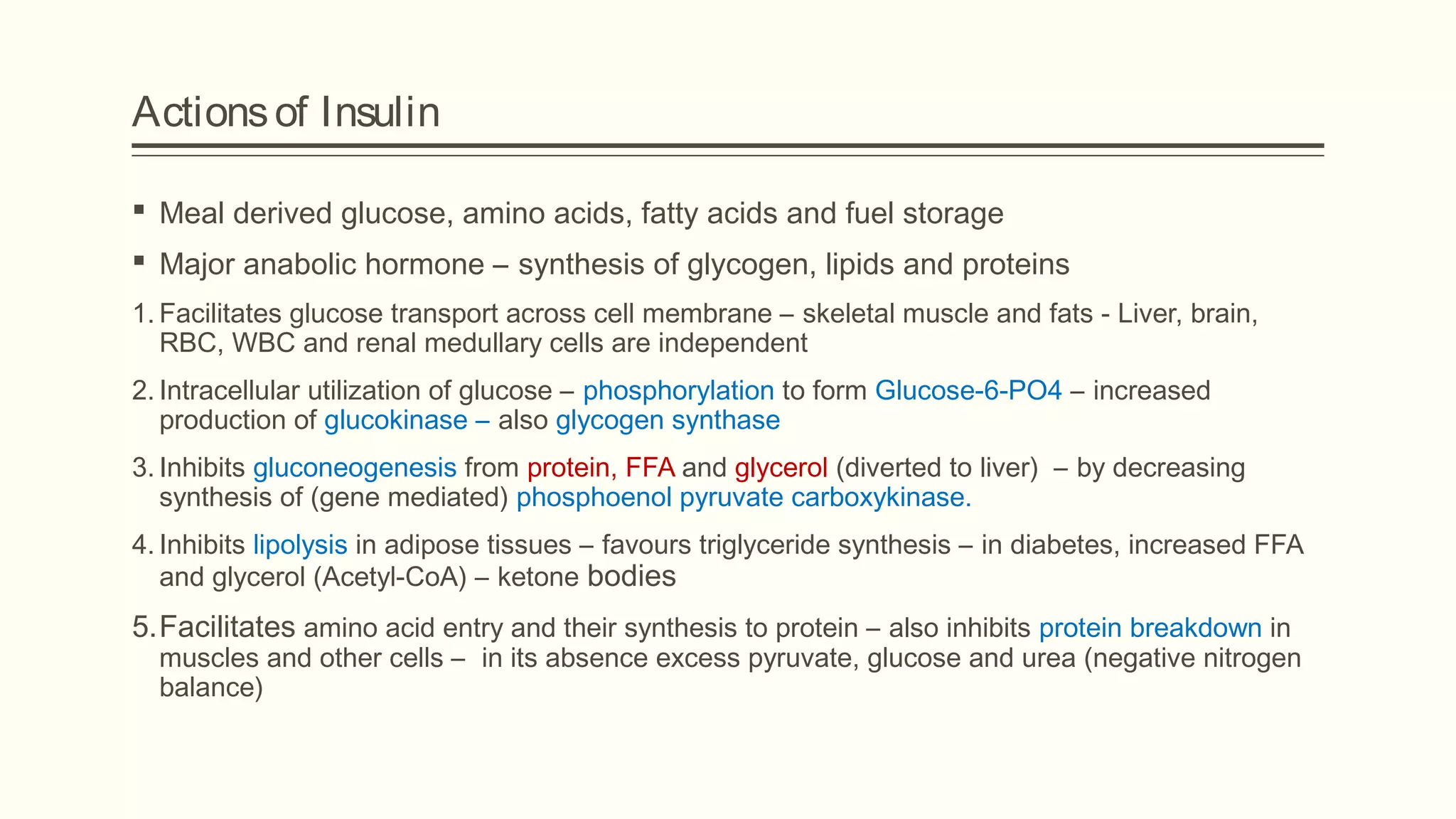
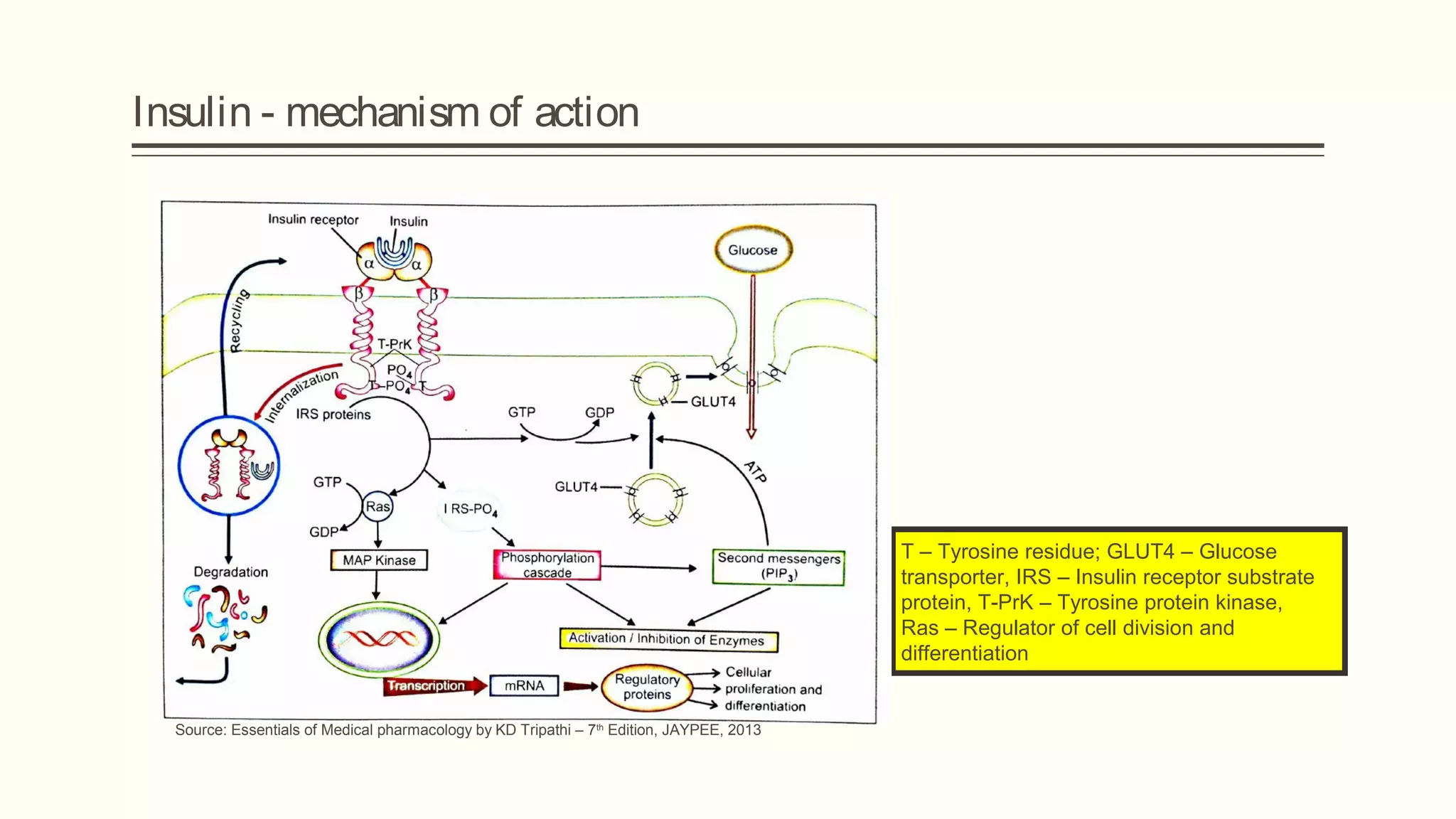
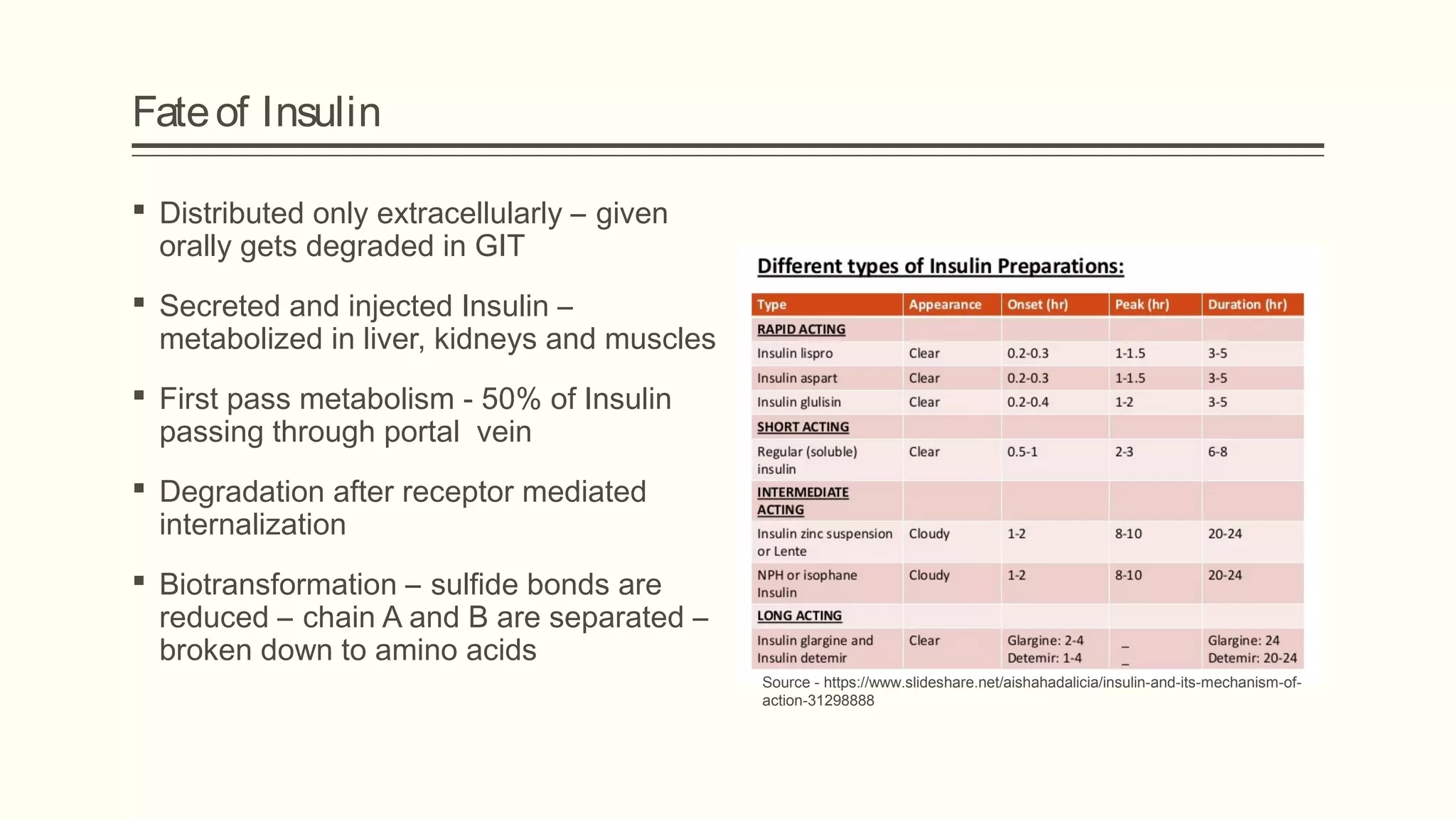
Insulin is a hormone produced in the pancreas that regulates blood sugar levels. It was discovered in 1921 and is used to treat diabetes by facilitating glucose entry into cells and inhibiting glucose production in the liver. There are various types of insulin preparations including regular, long-acting, and analogues produced through recombinant DNA technology to provide different durations of action.