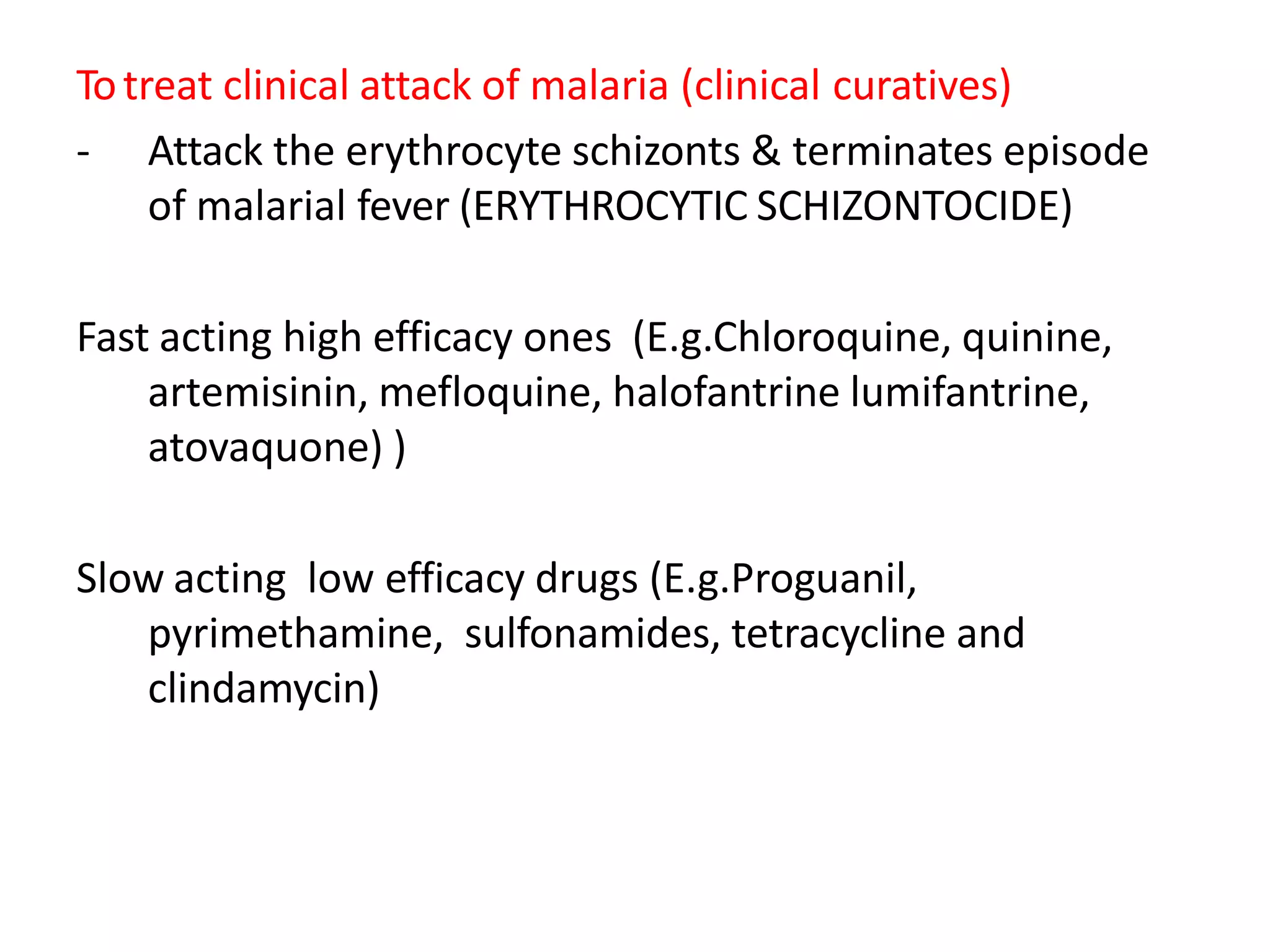
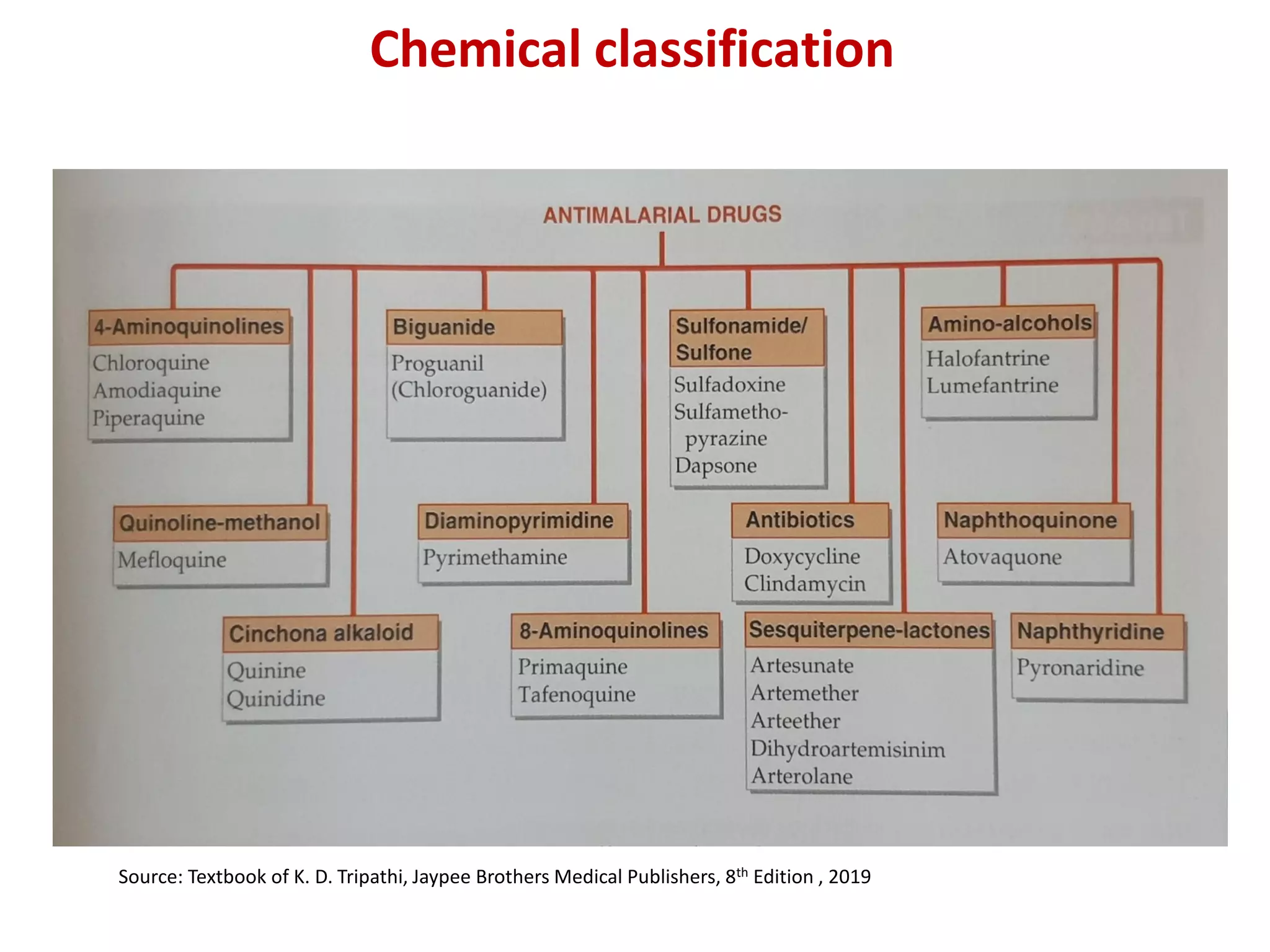
This document provides a comprehensive overview of antimalarial drugs, detailing the various species of Plasmodium causing malaria, their life cycle, and the classification of antimalarial drugs based on their therapeutic use. It discusses the objectives of these drugs, including prophylaxis, treatment, and radical cure, and highlights key medications such as chloroquine, mefloquine, and artemisinin derivatives along with their mechanisms of action, pharmacological effects, and adverse reactions. The document also addresses emerging drug resistance and the importance of combination therapy in effective malaria management.