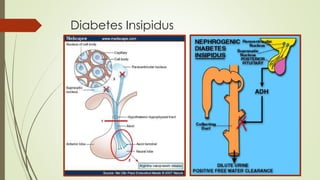
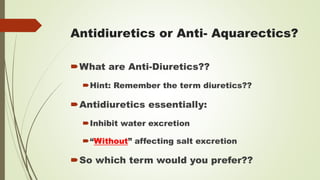
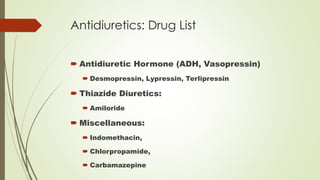
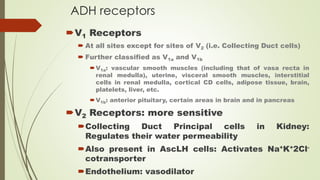
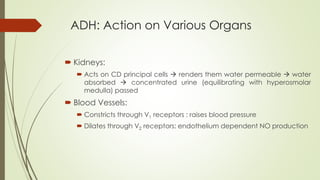
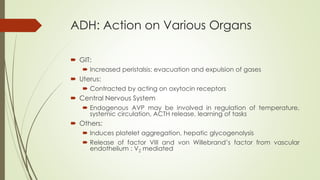
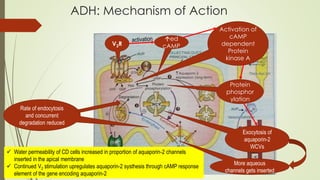
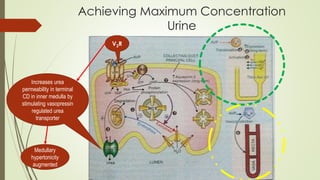
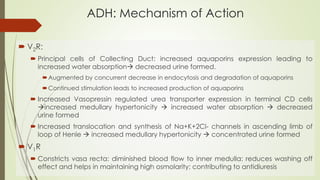
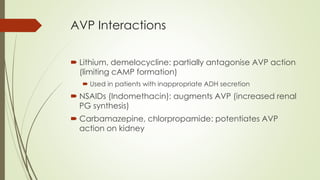
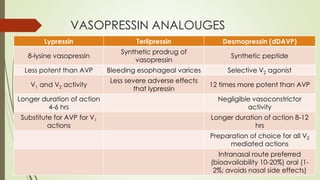
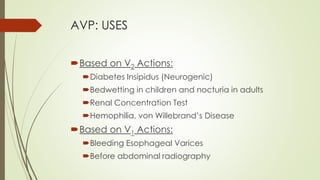
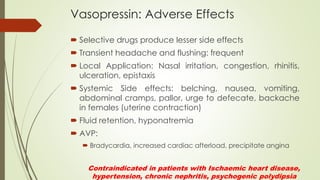
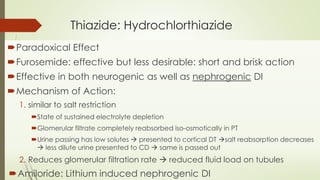
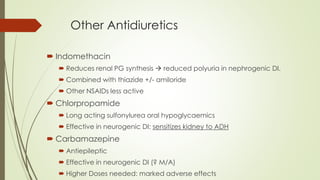
This document provides information about antidiuretic drugs. It begins by defining antidiuretics as drugs that inhibit water excretion without affecting salt excretion. It then lists common antidiuretic drugs including antidiuretic hormone, desmopressin, thiazide diuretics, and others. The document discusses the mechanism of action of antidiuretic hormone, its effects on various organs like the kidneys and blood vessels, and conditions it can be used to treat like diabetes insipidus. It also covers antidiuretic hormone receptors, interactions with other drugs, and potential adverse effects.