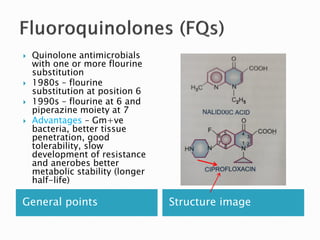
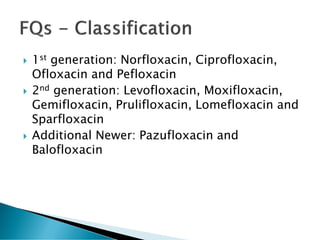
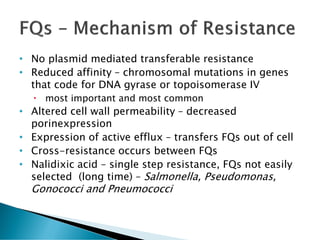
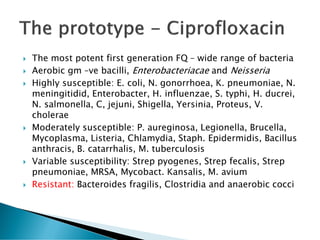
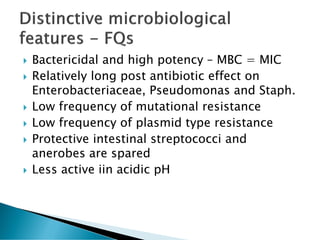
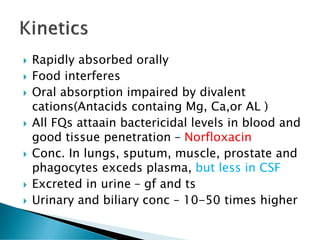
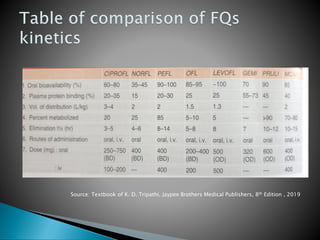
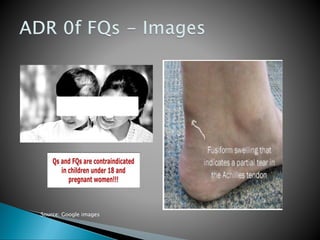
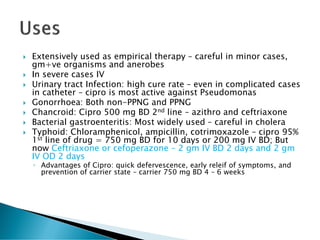
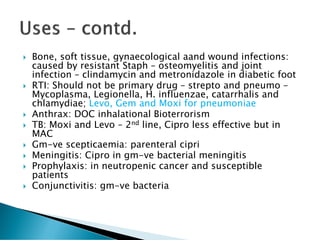
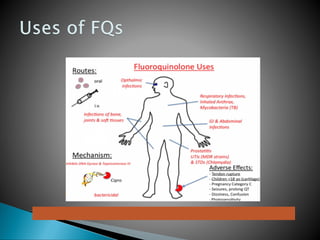
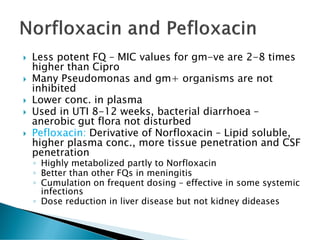
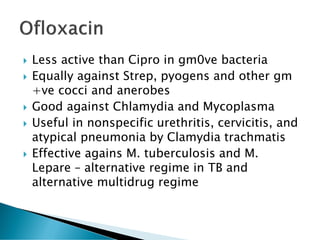
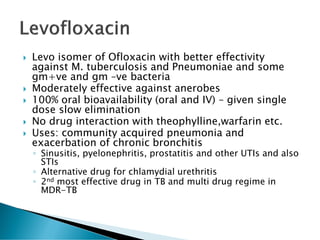
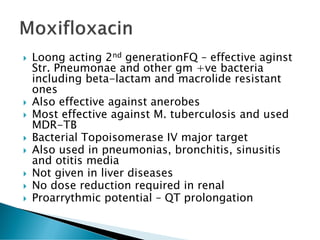
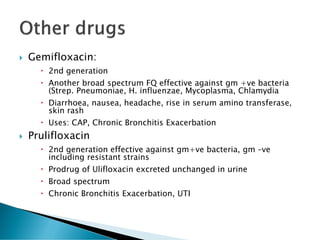
This document provides a comprehensive overview of quinolone antimicrobials, detailing their discovery, structure, mechanism of action, antibacterial spectrum, and resistance mechanisms. It discusses various generations of fluoroquinolones, their clinical uses, pharmacokinetics, and safety profile, highlighting their effectiveness against Gram-negative and Gram-positive bacteria. Additionally, it addresses the side effects and drug interactions associated with these medications, emphasizing the need for rational and cautious use in therapy.