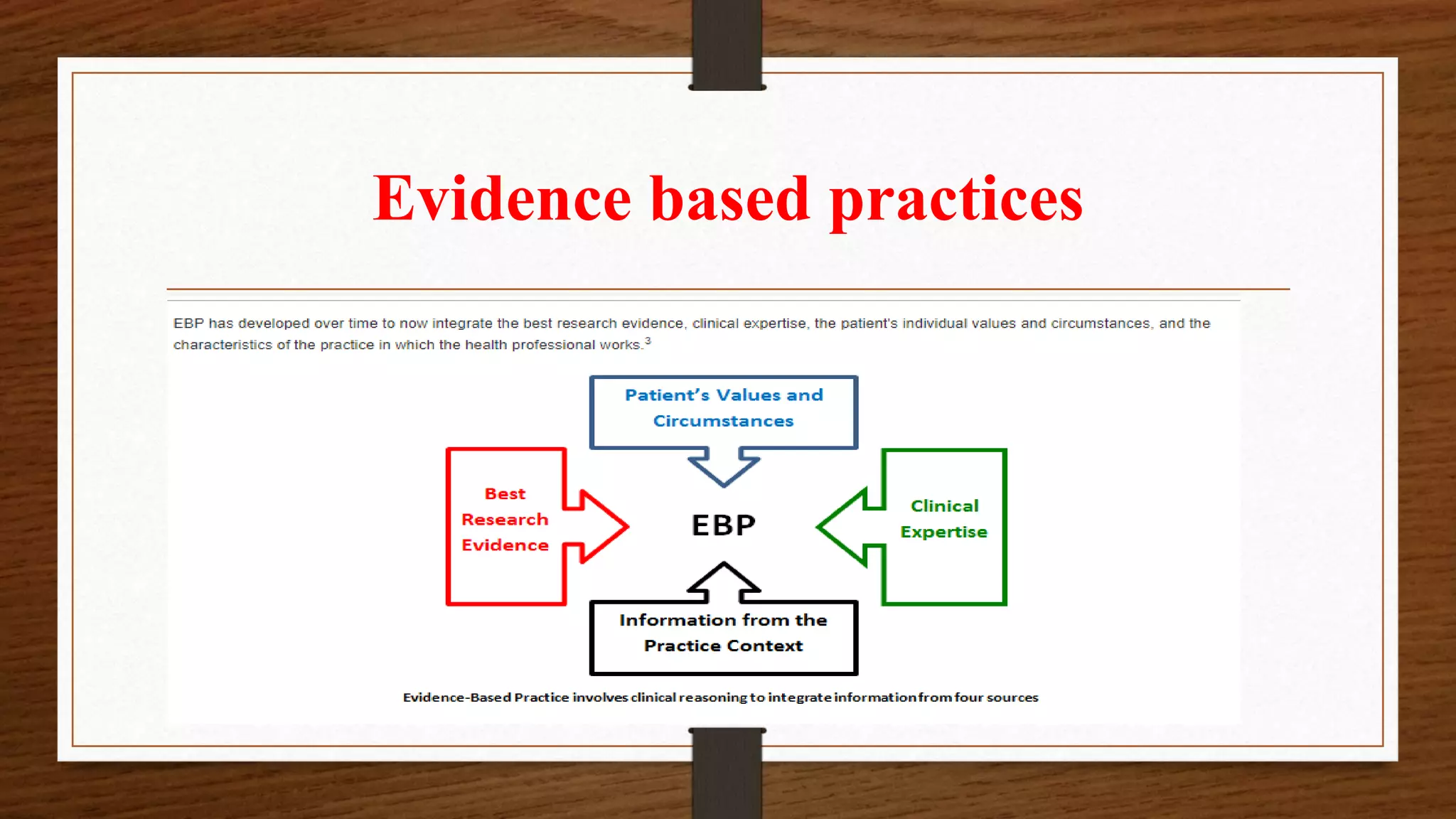
This document discusses evidence-based nursing practice. It begins by defining evidence-based practice as using the best available evidence from research, combined with clinical expertise and patient values, to achieve optimal patient outcomes. The goals of evidence-based practice are to maximize health and quality of life from the patient's perspective. The key components of evidence-based practice are research evidence, clinical expertise, and patient circumstances. The document also outlines the process of evidence-based practice, including formulating questions, searching literature, appraising evidence, applying evidence to practice, and evaluating outcomes.