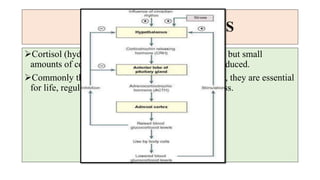
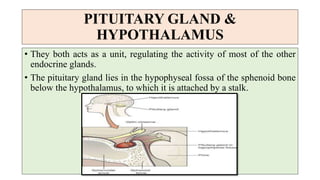
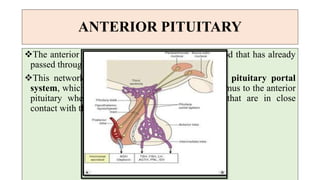
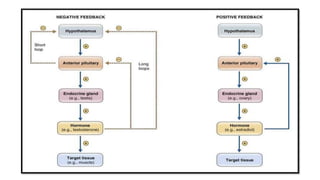
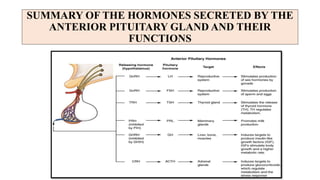
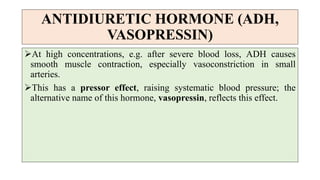
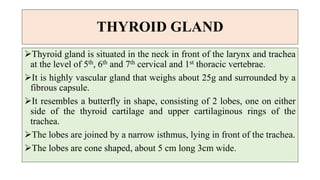
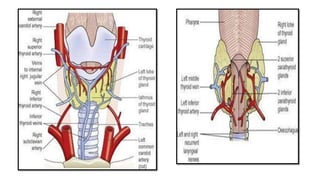
The document summarizes the key components and functions of the endocrine system. It describes the pituitary gland and hypothalamus as the central regulators of other endocrine glands. The pituitary gland has an anterior and posterior lobe, each producing distinct hormones. The hypothalamus controls pituitary hormone release through releasing and inhibiting hormones. The major hormones produced and their roles in growth, metabolism, reproduction and other processes are outlined.
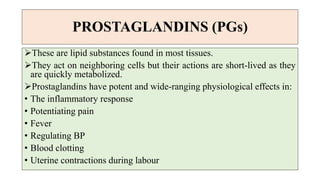
![ADRERNAL CORTEX
It produces 3 groups of steroid hormones from cholesterol
[adrenocorticoids (corticosteroids)]. These are:
1. Glucocorticoids
2. Mineralocorticoids
3. Sex hormones (androgens)](https://image.slidesharecdn.com/theendocrinesystem-210729062529/85/The-endocrine-system-43-320.jpg)