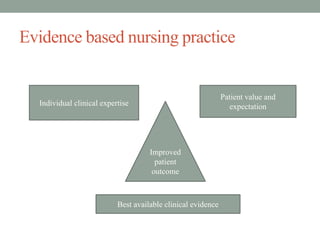
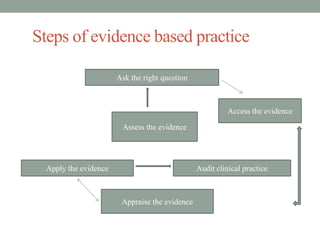
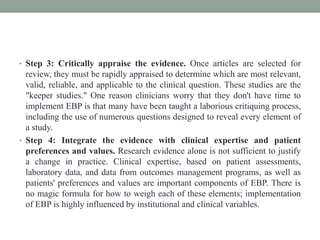
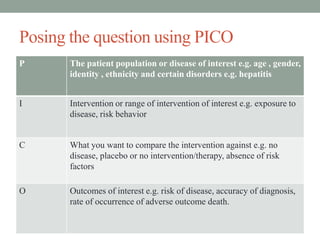
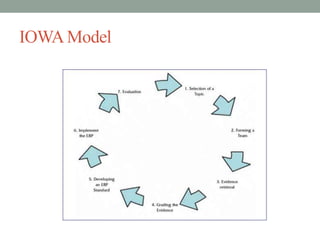
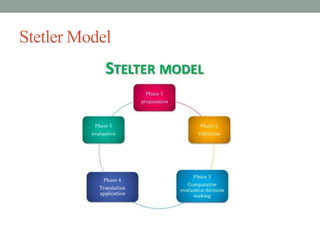
This document provides an overview of evidence-based practice (EBP) presented by Amritanshu Chanchal at Subharti Nursing College in Meerut. It defines EBP, discusses its components and key steps. The presentation covers asking questions using PICOT format, searching for evidence, critically appraising evidence, integrating evidence with clinical expertise and patient preferences, evaluating outcomes, and disseminating results. Models for EBP are also introduced, including the Iowa Model which outlines identifying triggers for change, determining organizational priority, and forming an interdisciplinary team to develop, evaluate and implement EBP changes.