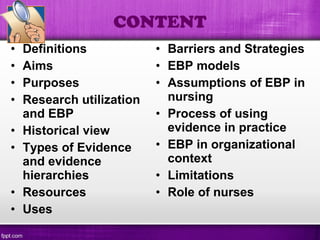
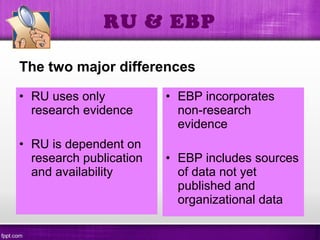
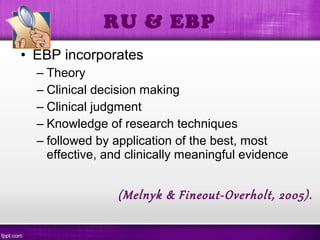
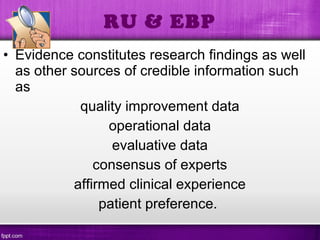
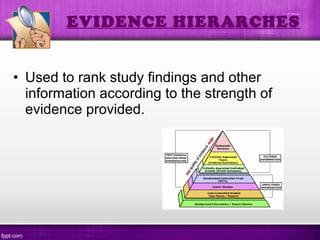
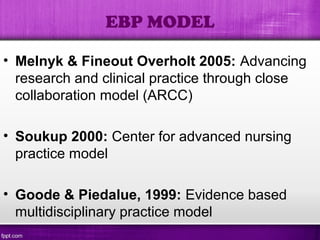
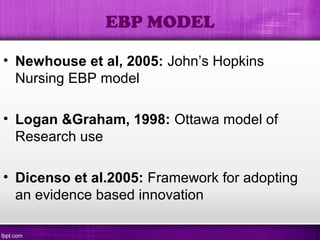
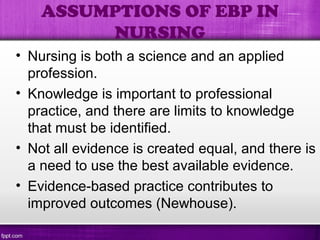
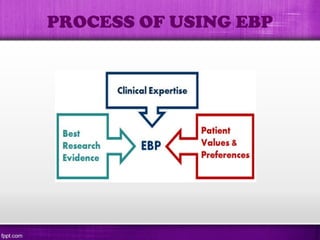
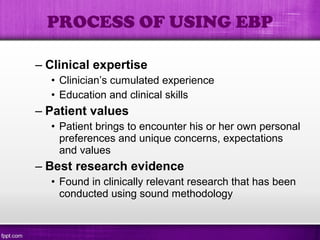
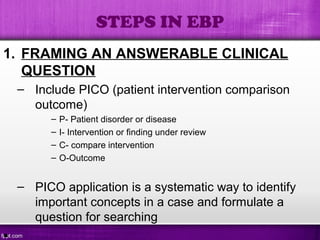
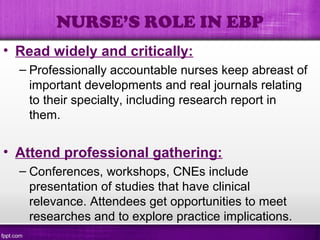
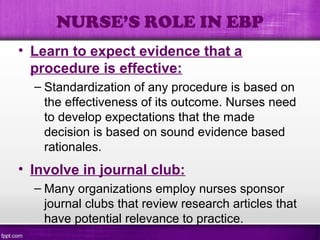
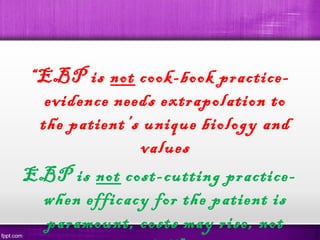
This document provides an overview of evidence-based practice (EBP) in nursing. It defines EBP and discusses its aims, purposes, and historical development. The document outlines the differences between EBP and research utilization and describes various types of evidence and hierarchies. It also identifies resources for EBP, discusses its uses and barriers, and presents several EBP models and the process of implementing EBP. The document notes assumptions of EBP in nursing, its limitations, and the role of nurses in EBP. Overall, the document serves as an introduction to EBP for nursing by defining key concepts and outlining the principles and process of EBP.