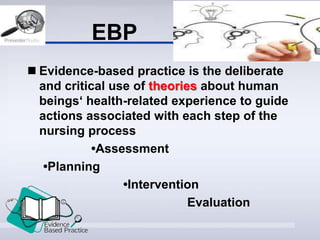
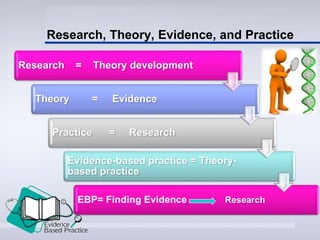
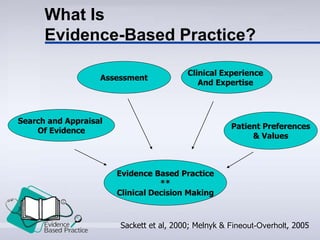
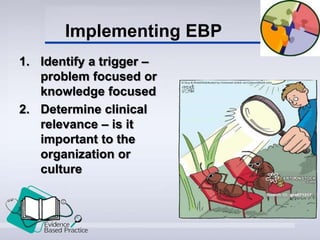
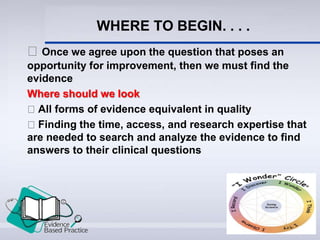
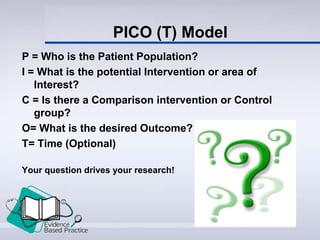
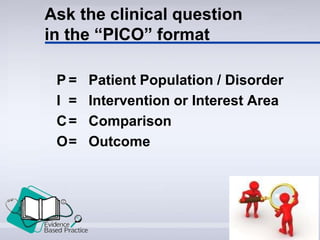
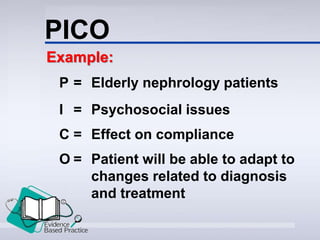
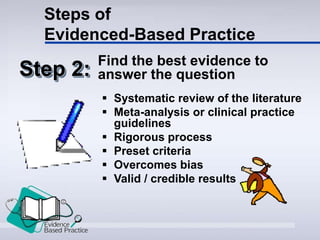
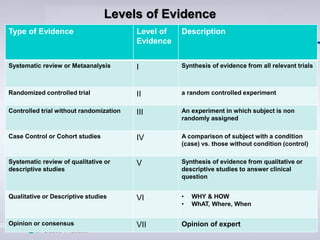
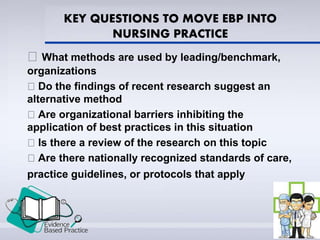
This document provides an introduction to evidence-based practice (EBP). It defines EBP as using the best available research evidence, along with clinical expertise and patient values, to guide patient care. The document discusses the history and importance of EBP, outlines the steps of EBP including framing clinical questions and searching for evidence, and identifies some barriers and facilitators to implementing EBP. The overall purpose is to familiarize readers with the core concepts and process of evidence-based practice in nursing.