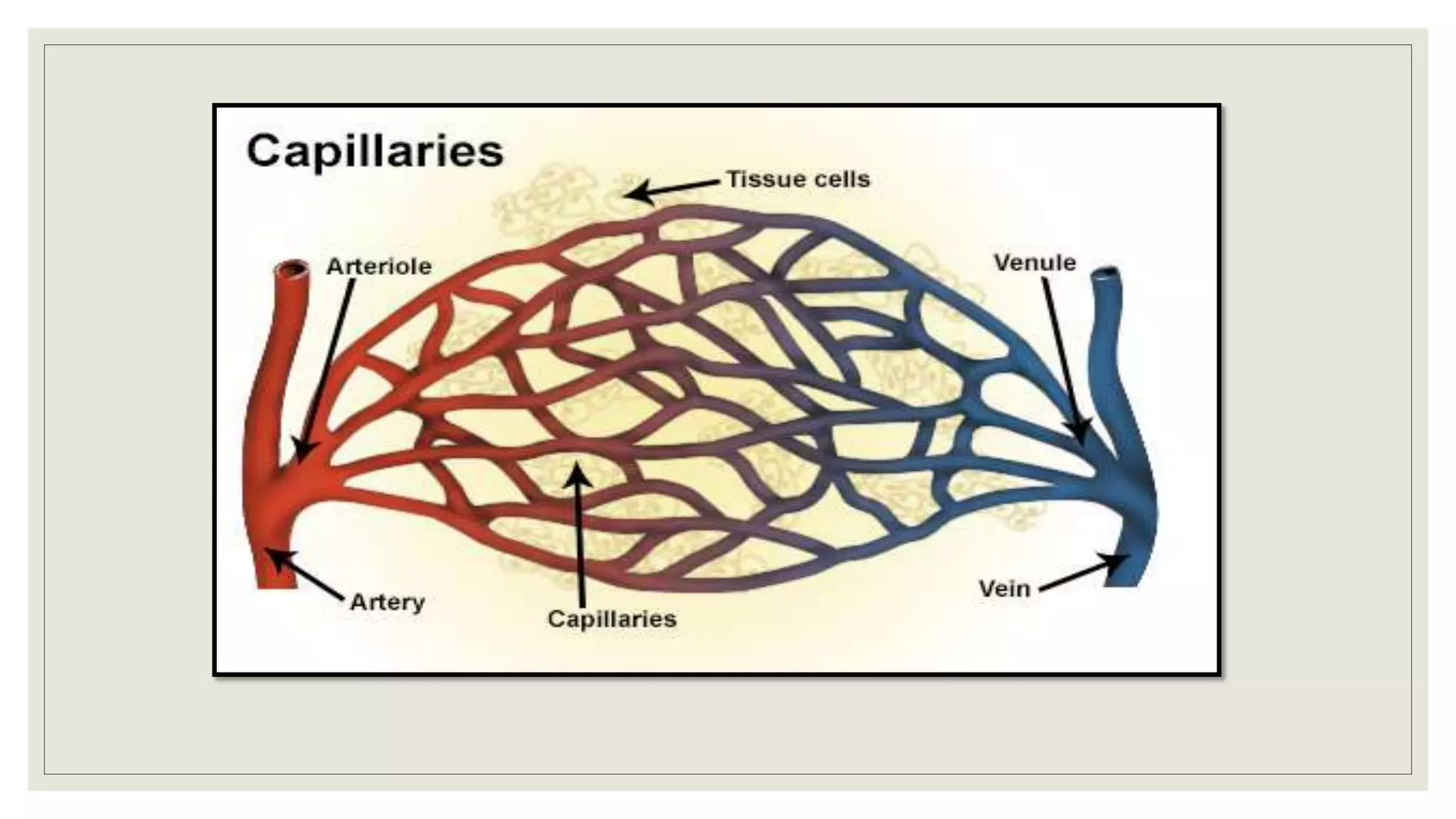
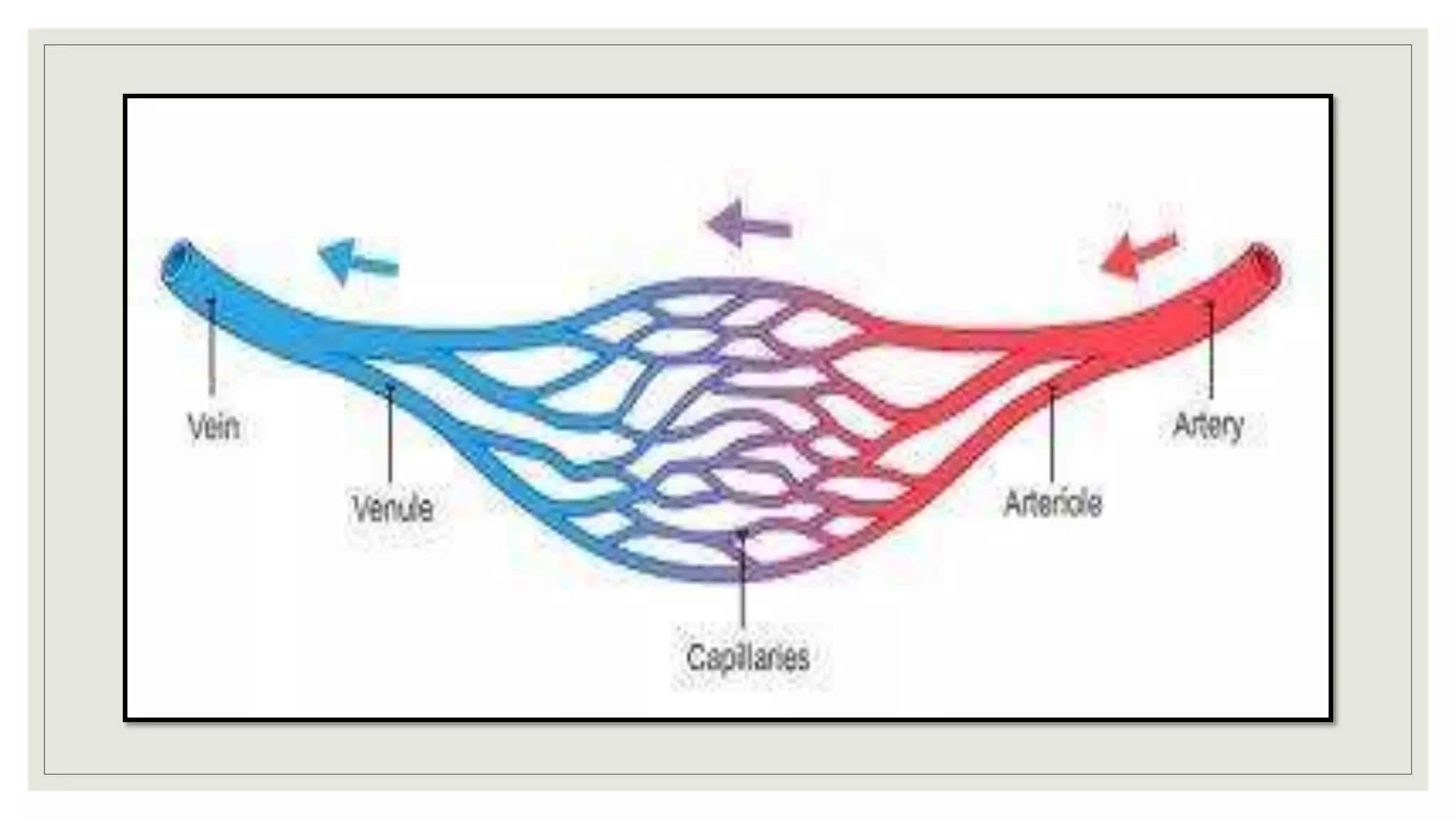
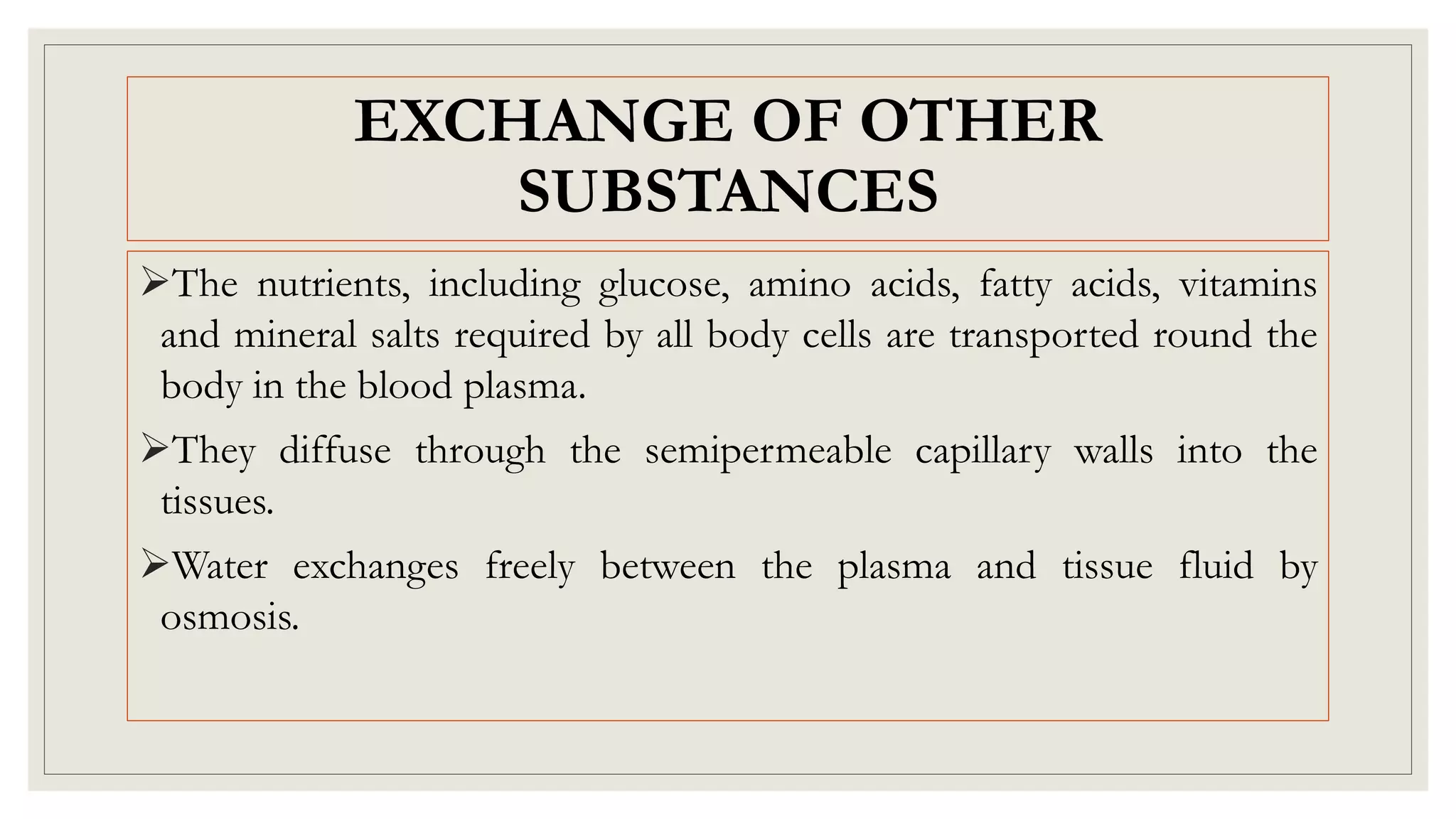
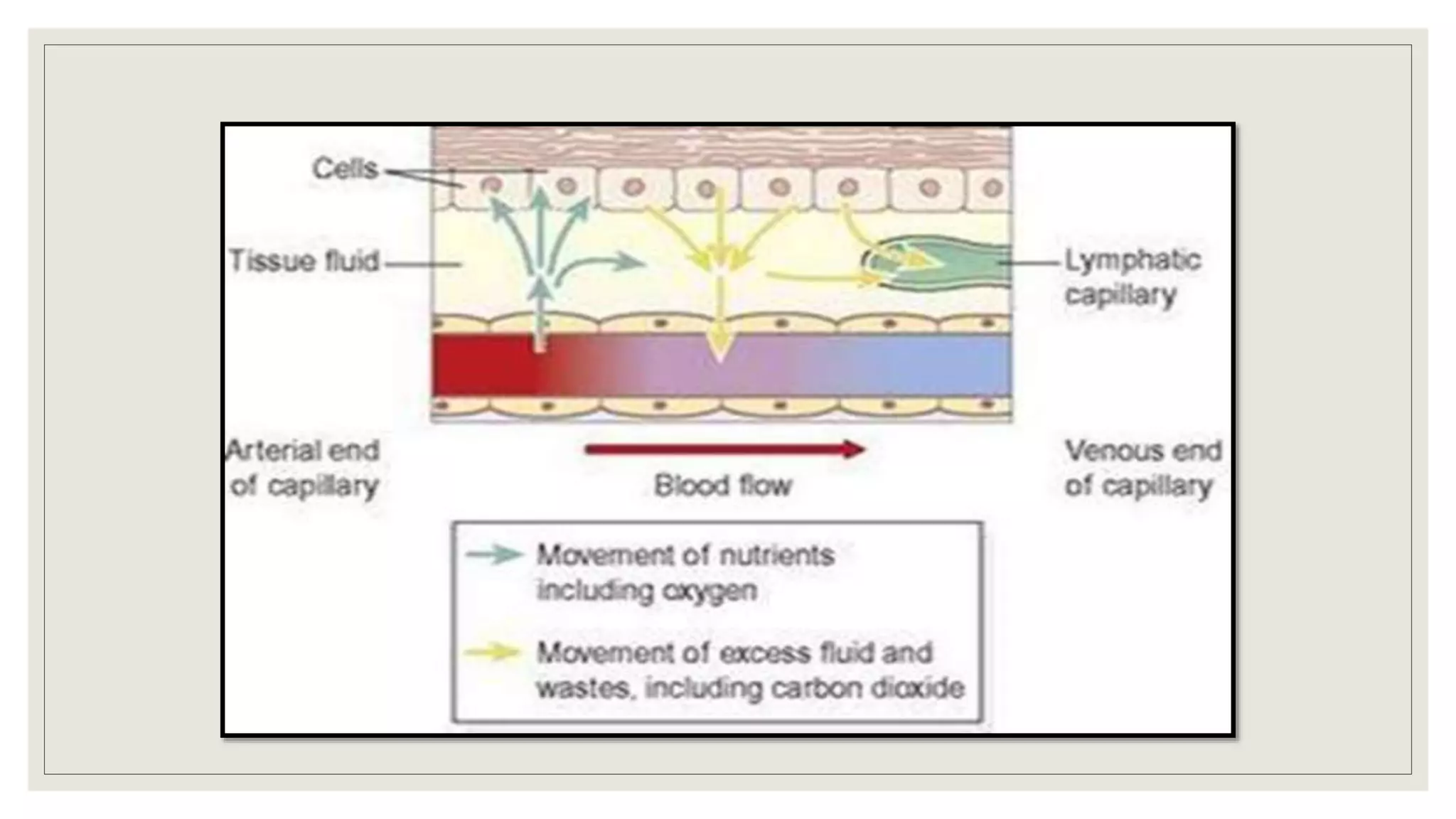
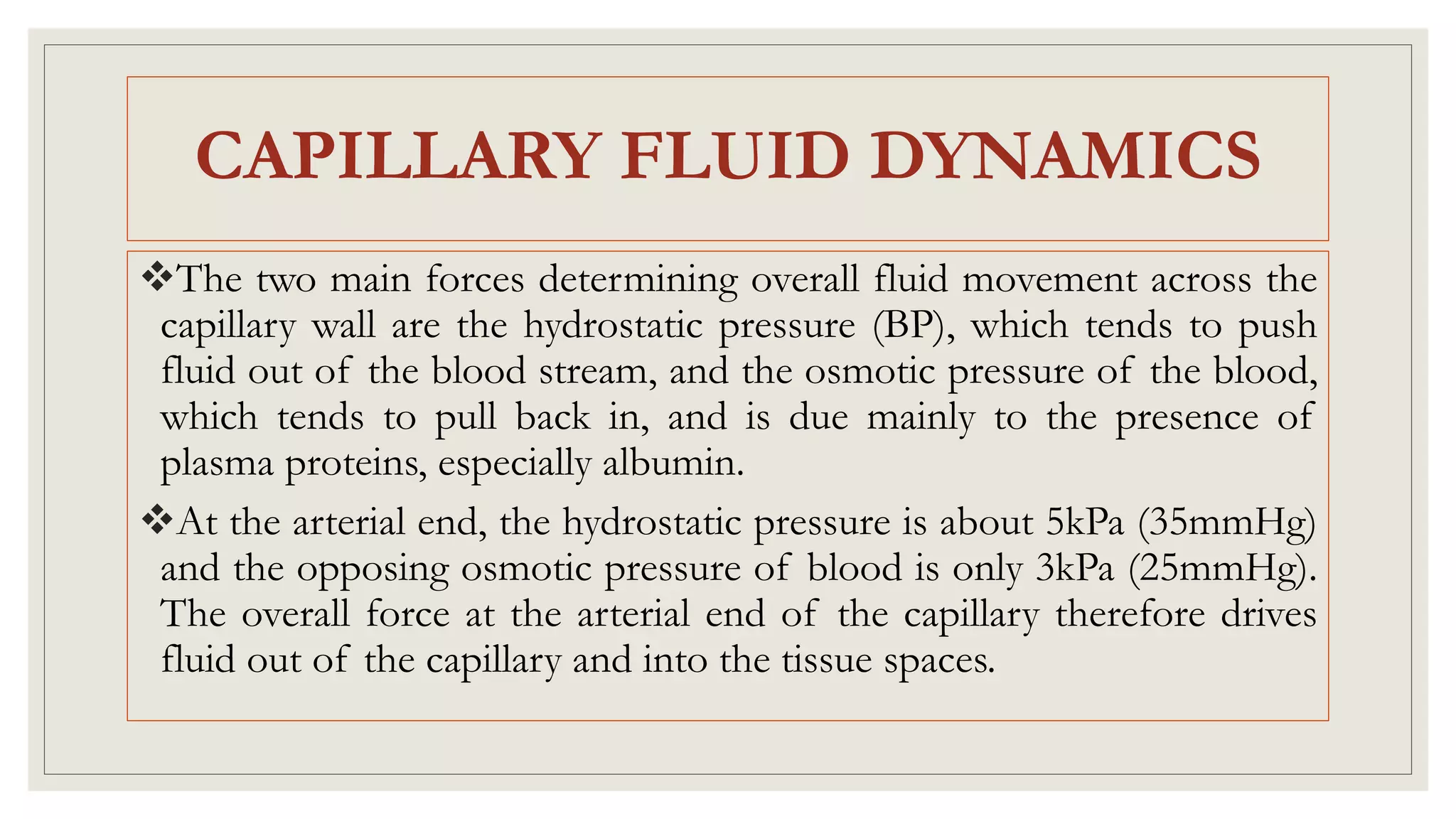
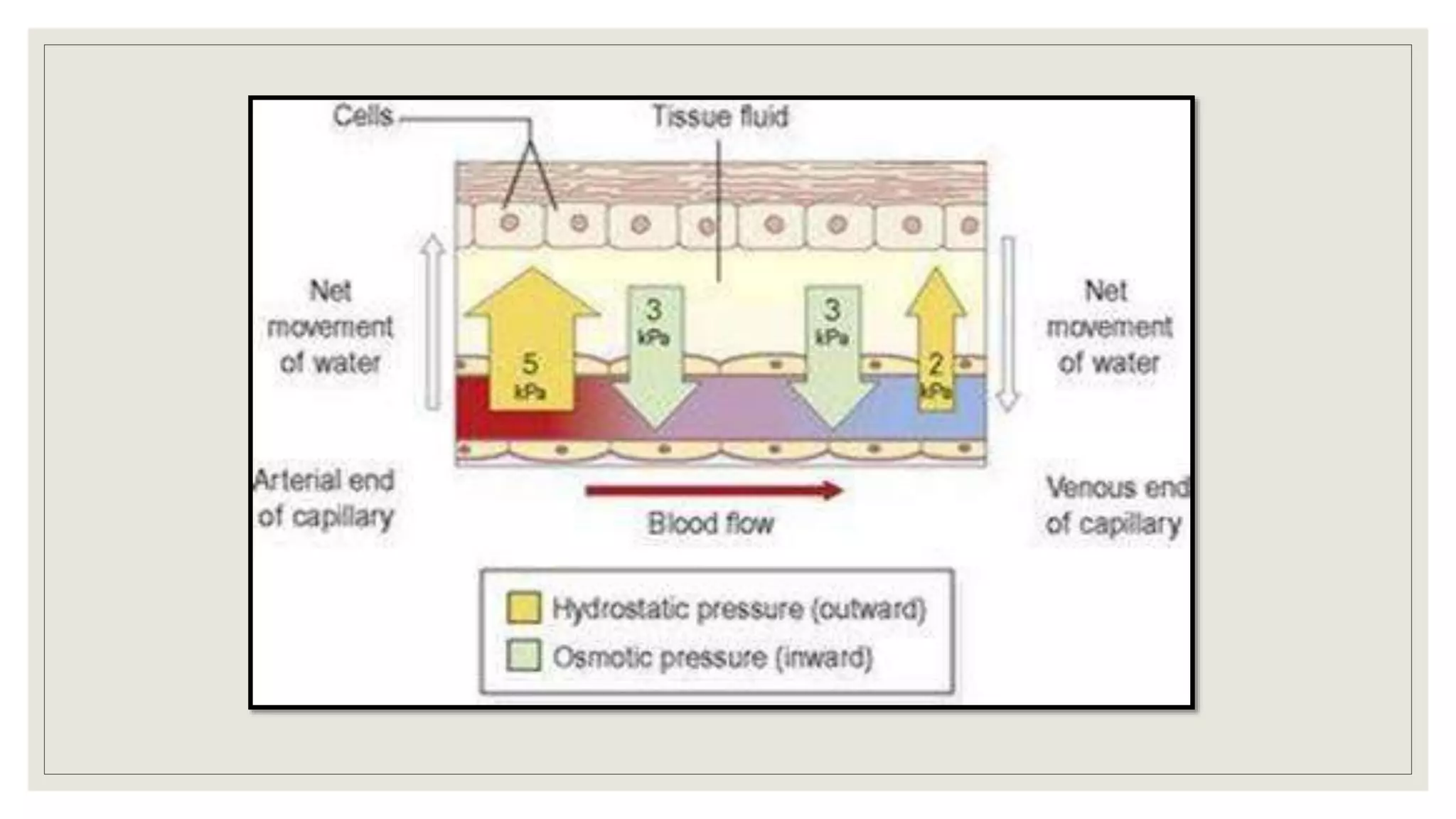
The document provides an overview of the cardiovascular system, detailing the structure and function of blood vessels, including arteries, arterioles, capillaries, venules, and veins. It explains how these vessels regulate blood flow and pressure through mechanisms like autoregulation and the impacts of sympathetic nervous system activity. Additionally, it describes the exchange of gases and other substances in capillaries and the dynamics of fluid movement across capillary walls.