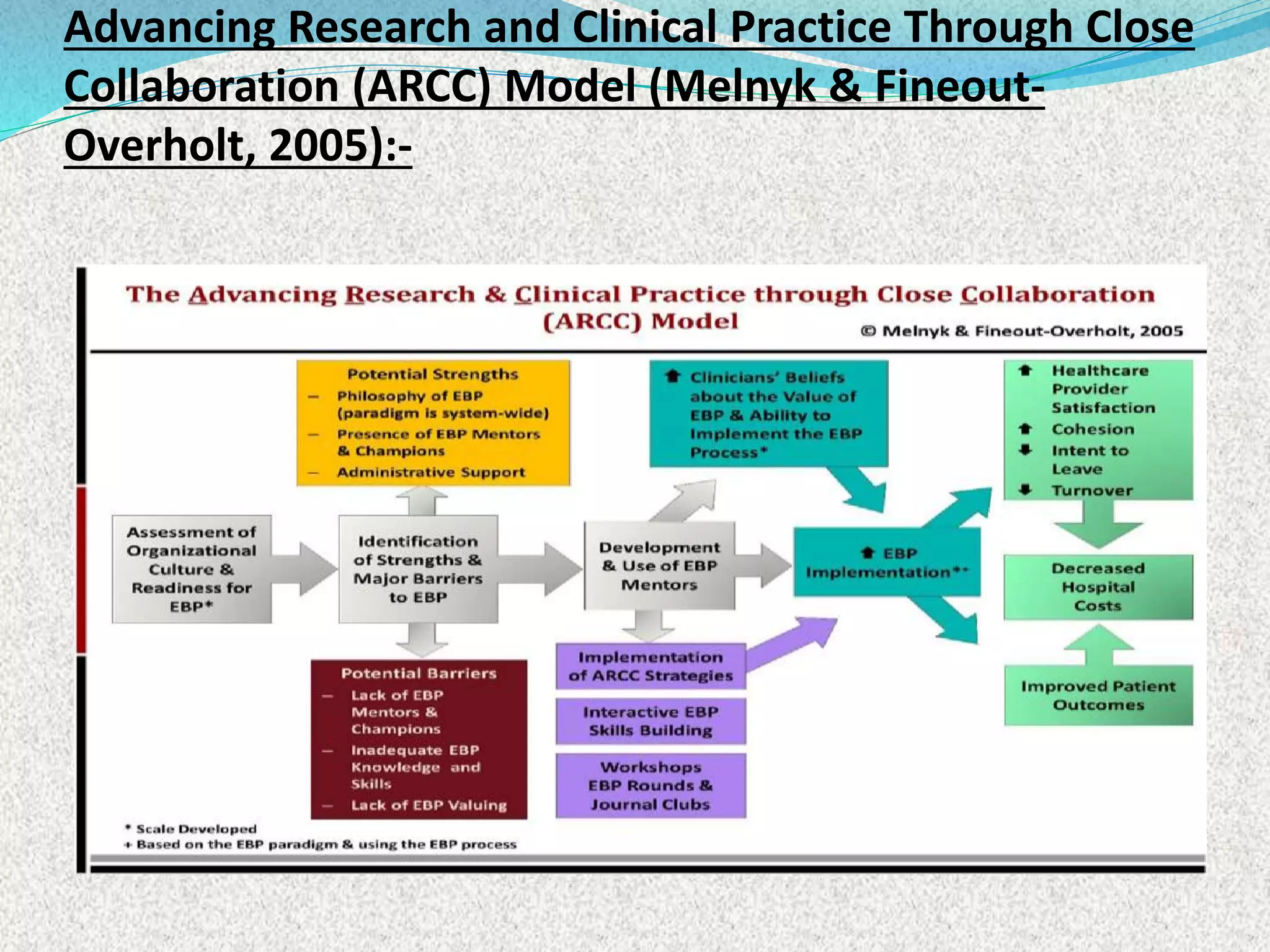
1. A U.S. study found that nurses reported low competency in evidence-based practice skills and identified factors like education level, EBP beliefs and mentorship as influencing competency.
2. A qualitative study found that patients accepted a pressure ulcer prevention care bundle when it encouraged participation through positive interactions with nurses and easy to understand information.
3. Interviews with hospital staff identified creating a supportive organization, maintaining awareness of prevention, and focusing on patient benefits as key factors for successful pressure ulcer prevention.