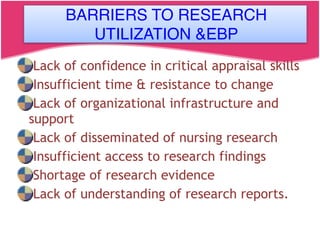
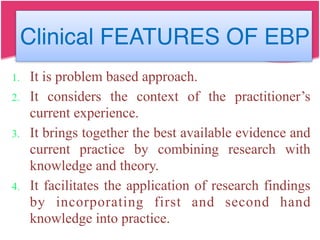
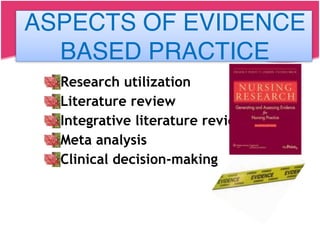
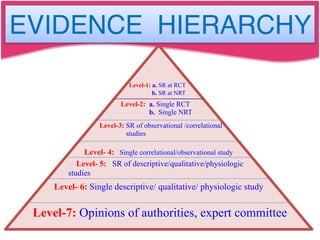
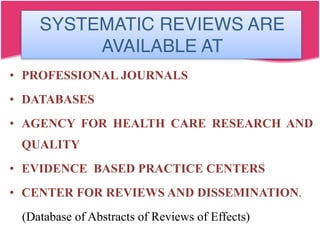
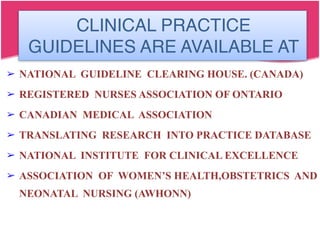
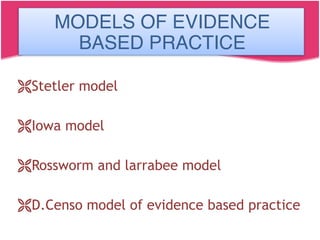
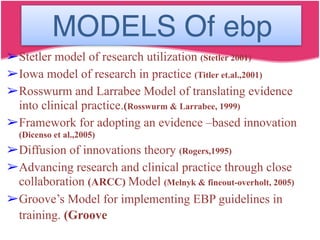
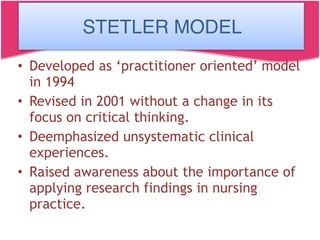
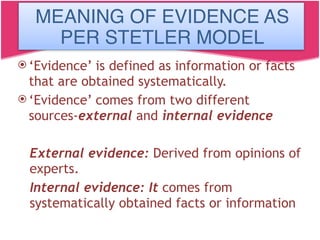
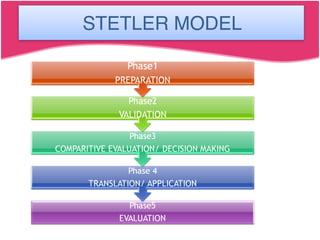
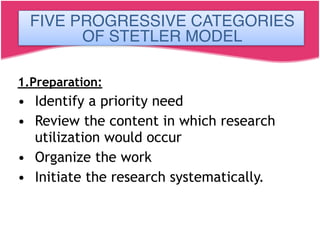
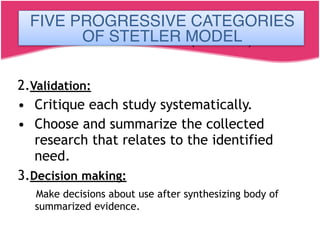
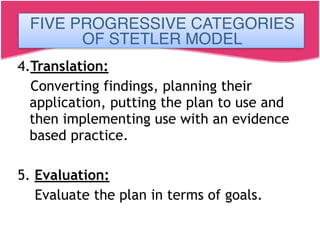
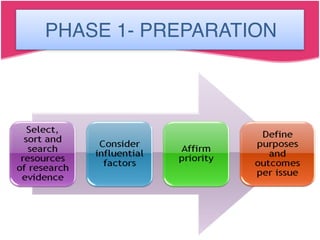
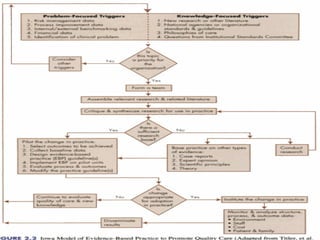
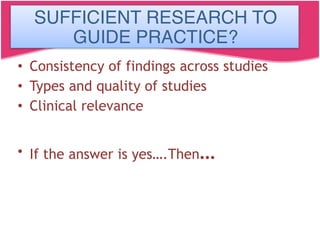
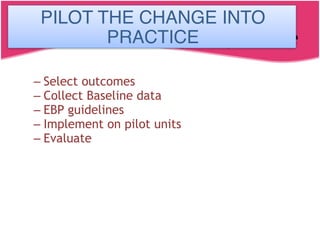
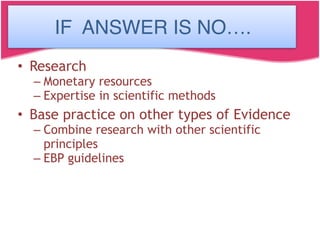
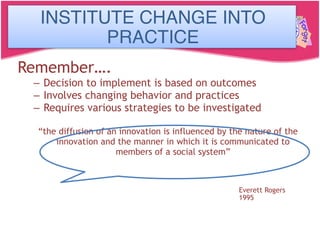
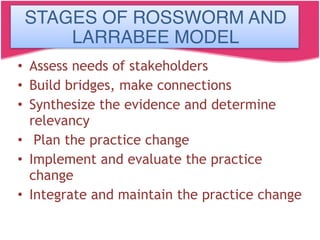
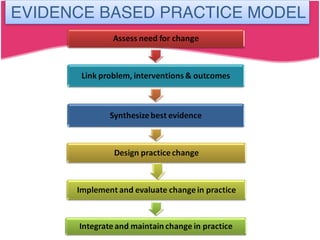
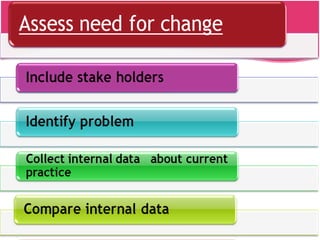
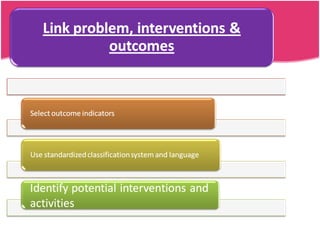
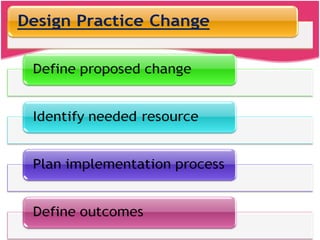
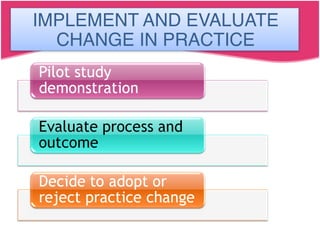
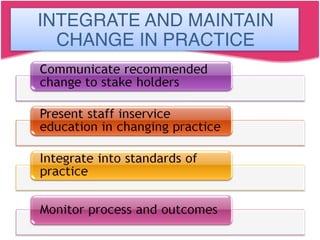
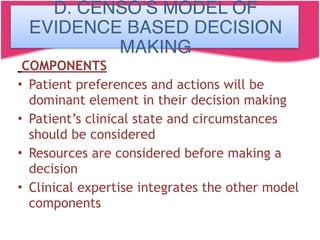
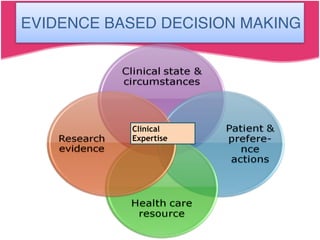
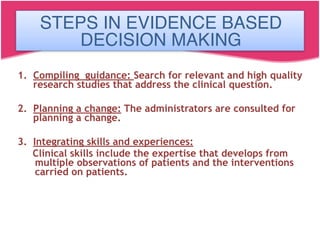
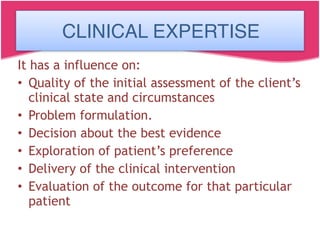
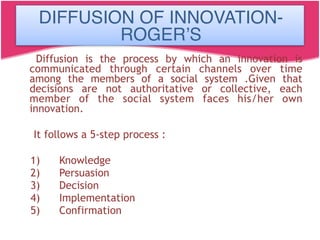
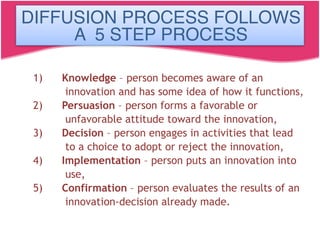
The document discusses evidence based nursing practice. It defines nursing research, evidence, evidence based decision making and evidence based practice. Evidence based nursing practice refers to using the best research evidence, clinical expertise and patient preferences in clinical decision making. The evidence based practice movement started in the 1990s to improve care quality. Models like the Stetler model and Iowa model provide frameworks for evidence based practice. Barriers to evidence based practice include lack of time, skills and research access. Guidelines and systematic reviews are sources of best evidence.