1. Venous thromboembolic diseases that can occur during pregnancy and postpartum include deep vein thrombosis, thrombophlebitis, and pulmonary embolism.
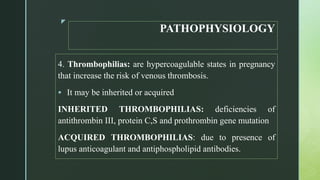
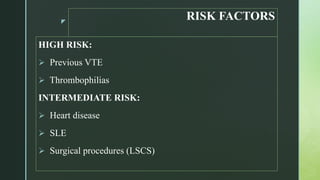
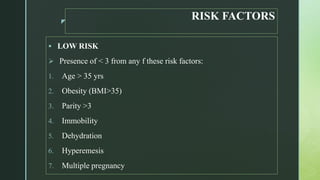
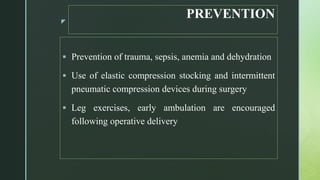
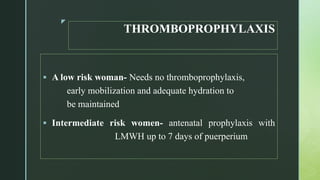
2. Risk factors for these conditions include inherited or acquired thrombophilias, previous VTE, heart disease, surgery such as C-section, age over 35, obesity, multiple pregnancy, and immobility.
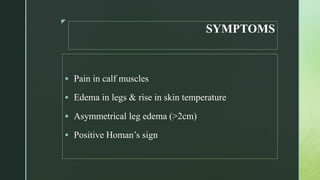
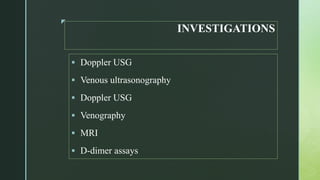
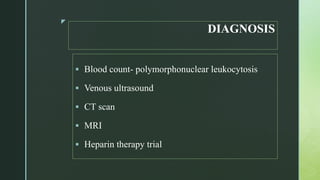
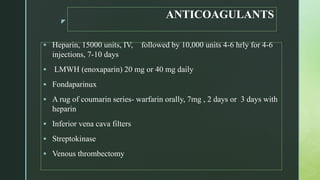
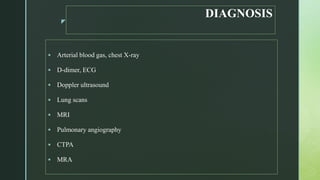
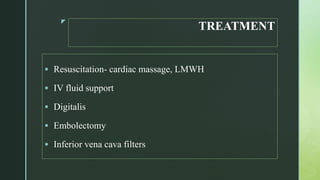
3. Diagnosis involves Doppler ultrasound, venous ultrasonography, or CTPA. Treatment consists of anticoagulants like heparin or LMWH, thrombectomy, or inferior vena cava filters to prevent further embolism.