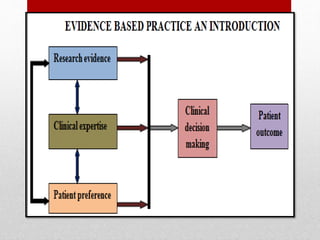
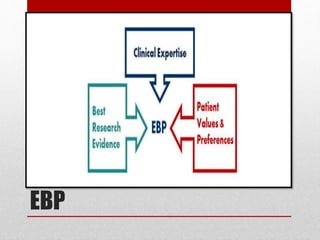
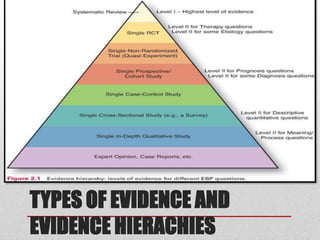
The presentation outlines evidence-based practice (EBP) in healthcare, defining it as the judicious use of current best evidence for patient care. It emphasizes the importance of integrating research findings into nursing practice and describes the steps involved in EBP, from formulating clinical questions to appraising and implementing evidence. Additionally, it highlights barriers to research utilization and various models that guide the application of evidence in nursing.