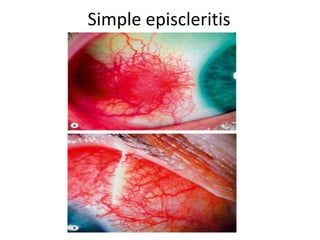
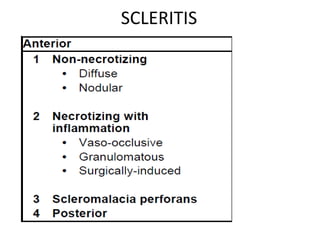
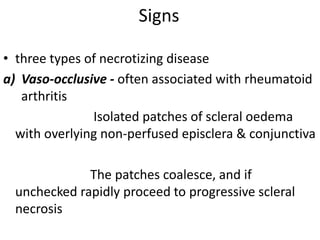
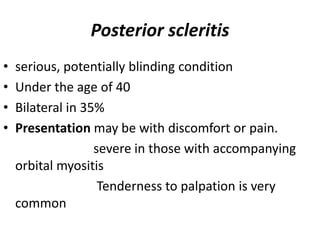
Scleritis and episcleritis affect the layers of the sclera and surrounding tissues. Episcleritis is usually benign and recurrent, occurring as either simple or nodular types. Scleritis can be anterior and non-necrotizing, nodular, or necrotizing. Complications of scleritis include keratitis, uveitis, glaucoma, hypotony, and perforation. Treatment involves topical steroids, NSAIDs, immunosuppressants, or antibiotics depending on the type and cause.