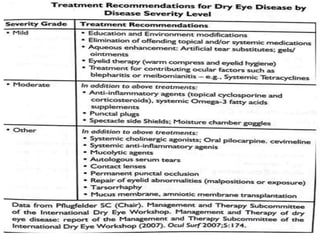
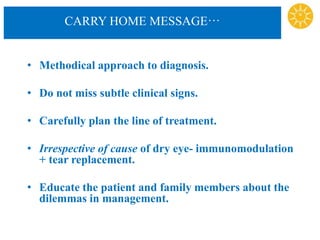
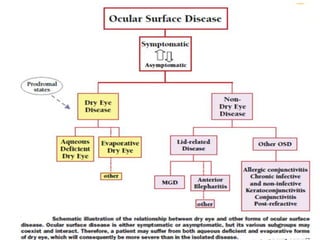
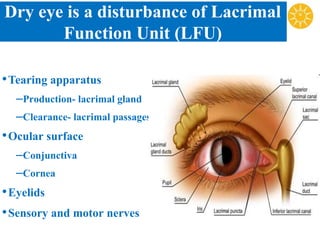
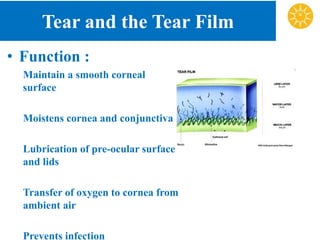
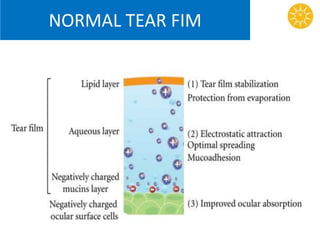
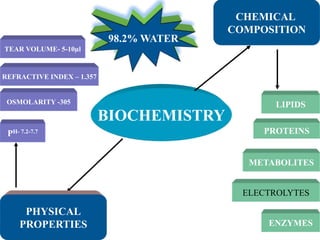
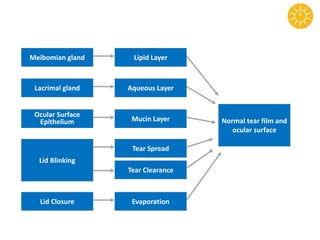
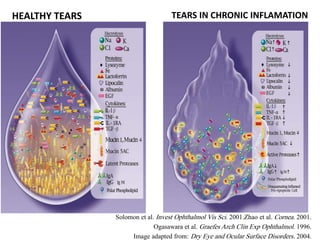
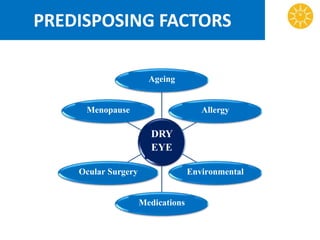
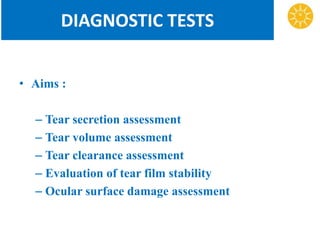
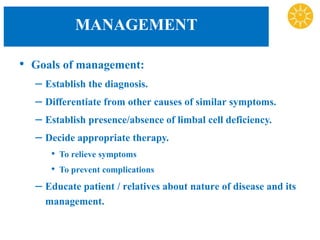
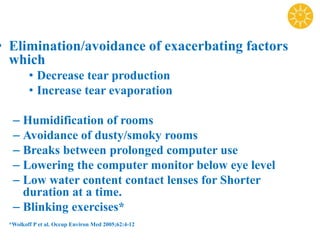
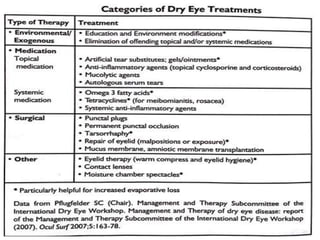
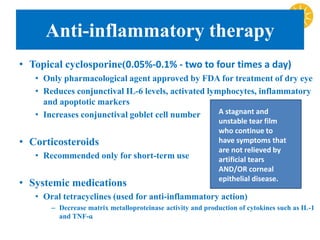
Dry Eye Disease is a multifactorial disease that results in discomfort and visual disturbances due to tear film instability and inflammation of the ocular surface. It is caused by a disturbance in the lacrimal functional unit involving tear production, distribution, and clearance. Diagnosis involves evaluating tear secretion, volume, and stability as well as assessing ocular surface damage. Management focuses on eliminating exacerbating factors, supplementing tears, anti-inflammatory therapy, punctal plugs, and newer treatments targeting tear stimulation and mucous secretion when needed.

![INTRODUCTION
• Dry eye is a multifactorial disease of the tears
and the ocular surface that results in symptoms
of discomfort, visual disturbance, and tear film
instability with potential damage to then ocular
surface.
• accompanied by increased osmolarity of the tear
film and inflammation of the ocular surface
*2007 Report of the Dry Eye Work Shop (Ocul Surf 2007;5[2]:65-204)](https://image.slidesharecdn.com/ded-150702174841-lva1-app6892/85/Dry-eyes-3-320.jpg)
![*2007 Report of the Dry Eye Work Shop (Ocul Surf 2007;5[2]:65-204)](https://image.slidesharecdn.com/ded-150702174841-lva1-app6892/85/Dry-eyes-12-320.jpg)



![Newer treatment modalities
• Mucolytic agents as
acetylcysteine 5% drops
used in patients with
corneal filaments and
mucous plaques.
• Autologous serum
drops [diluted 1:3 with
saline] have reported to
reduce ocular irritation
and conjuntival and
corneal dye staining in
Sjogren’s syndrome
associated aqueous tear
deficiency.](https://image.slidesharecdn.com/ded-150702174841-lva1-app6892/85/Dry-eyes-58-320.jpg)