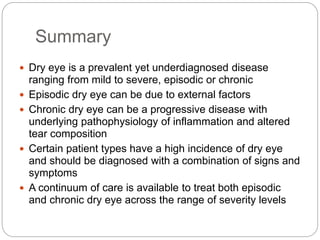
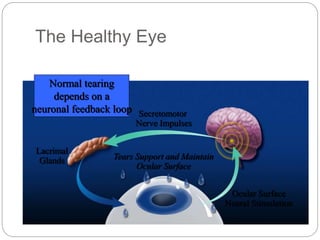
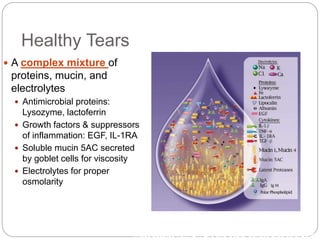
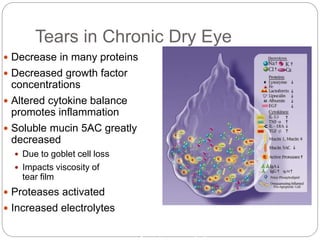
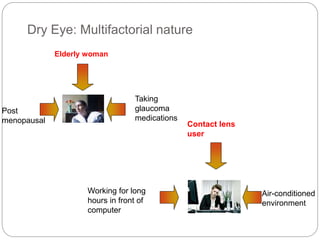
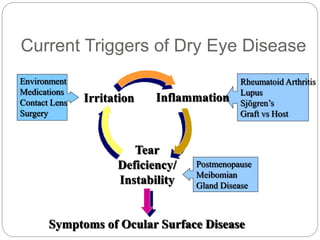
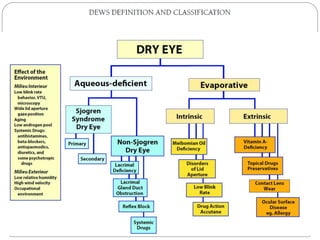
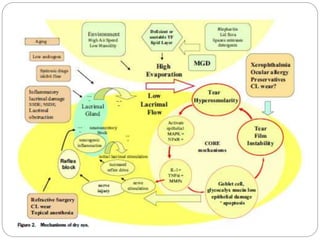
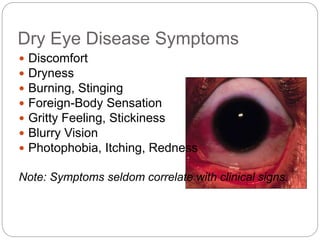
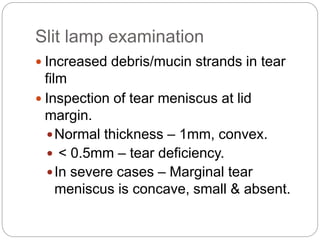
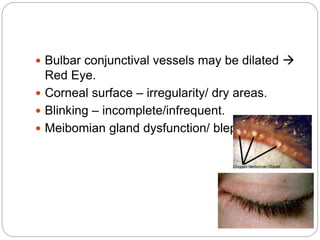
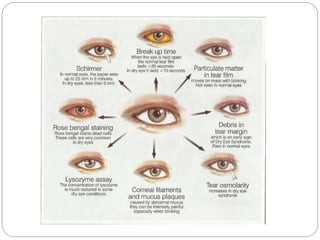
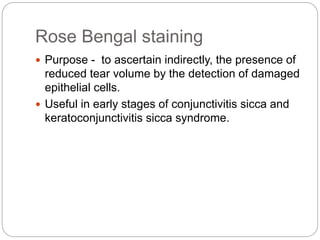
Dry eye disease (DED) is a multifactorial condition characterized by inflammation leading to tear film instability, causing discomfort and visual disturbances. It affects various demographics, particularly elderly women and contact lens users, with symptoms ranging from dryness to burning sensations. Diagnosis involves clinical tests including tear secretion measurements and staining techniques, while management options focus on alleviating symptoms and addressing underlying causes.

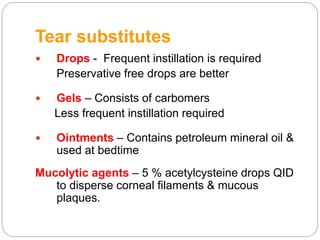
![Drops
Cellulose derivatives –
o Hydroxypropyl methylcellulose
o Carboxymethylcellulose [more useful in lipid or
mucous deficiency]
o Appropriate for mild cases.
Polyvinyl alcohol – Better in aqueous deficiency
o Dose
QID in mild cases
½ hrly – 2 hrly in severe cases
Sodium hyaluronate
Povidone
Sodium chloride
Hypromellose](https://image.slidesharecdn.com/dryeyefinal-151126071201-lva1-app6891/85/Dry-Eye-Disease-70-320.jpg)
![Other options
Topical cyclosporine [0.05%, 0.1%]
Reduces cell-mediated inflammation of lacrimal tissue
increase in goblet cells, reversal of squamous metaplasia of
conjunctiva.
Oral cholinergic agents (M3) like pilocarpine ,
cevimeline
Effective in xerostomia & about 40% of KCS patients also
obtain relief
Botulinum toxin injection to orbicularis muscle –
controls blepharospasm in severe dry eye.
Sub-mandibular gland transplantation – for
extreme dry eye.](https://image.slidesharecdn.com/dryeyefinal-151126071201-lva1-app6891/85/Dry-Eye-Disease-75-320.jpg)