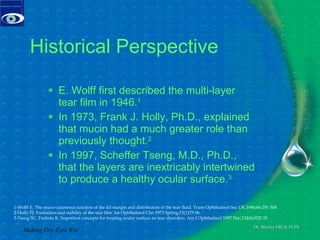
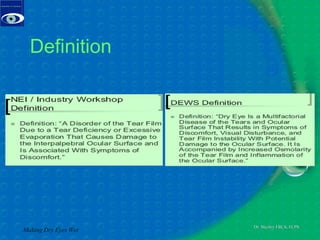
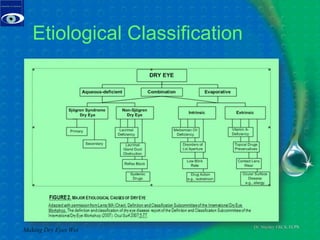
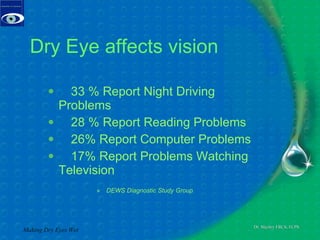
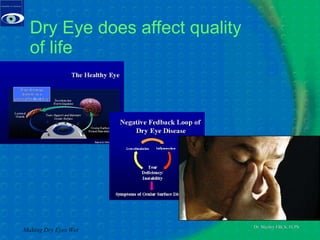
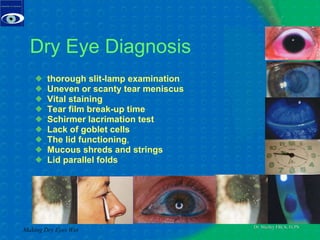
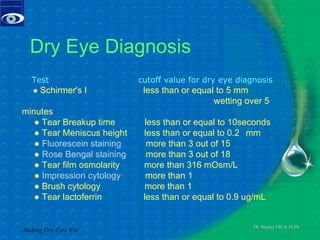
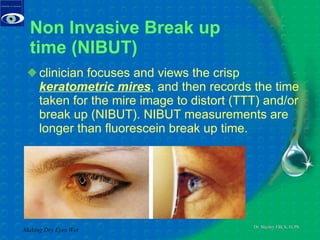
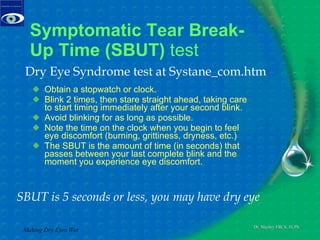
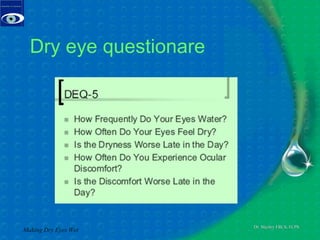
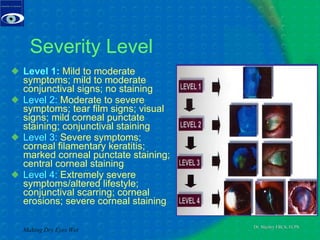
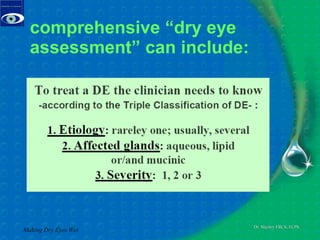
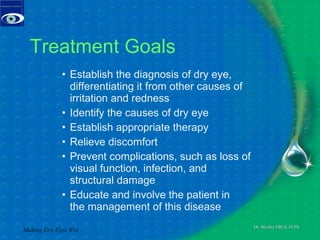
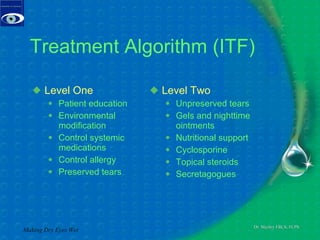
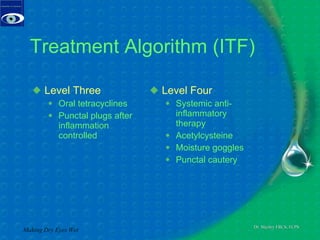
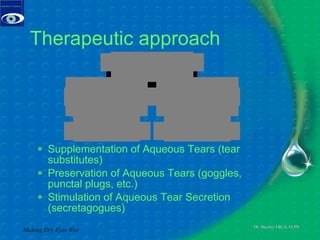
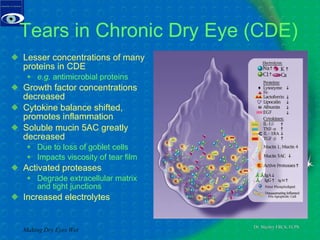
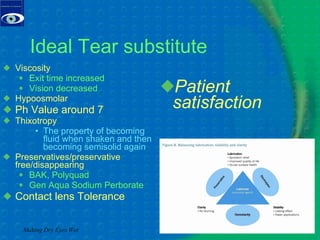
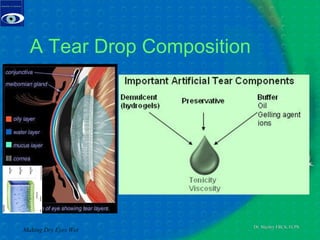
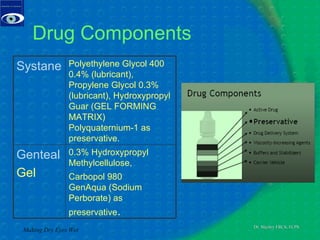
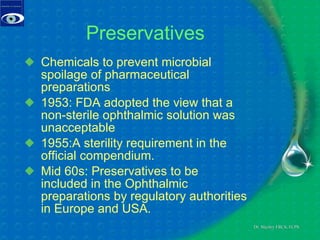
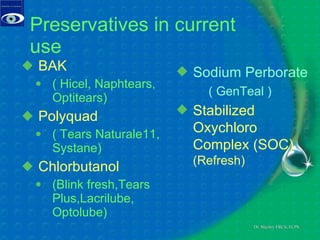
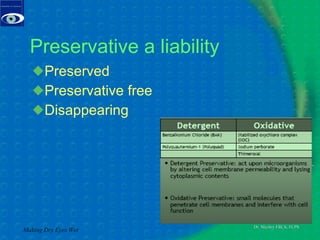
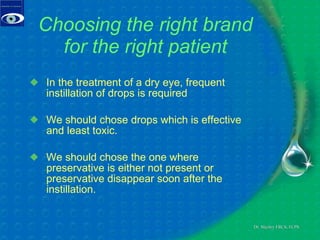
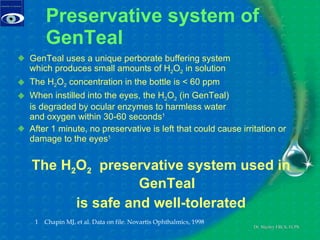
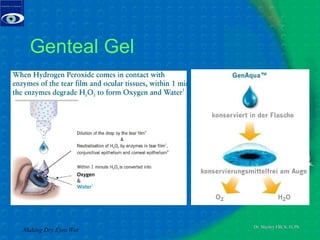
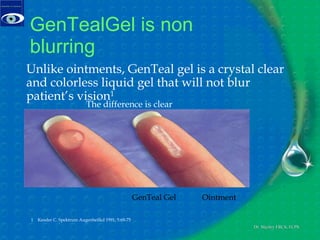
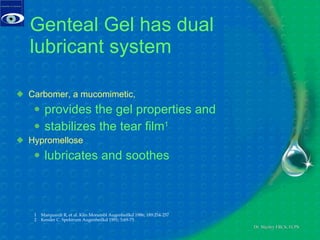
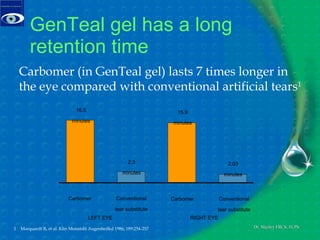
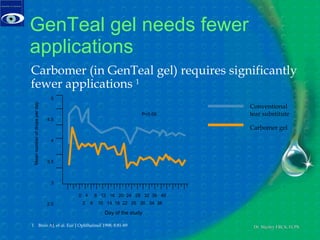
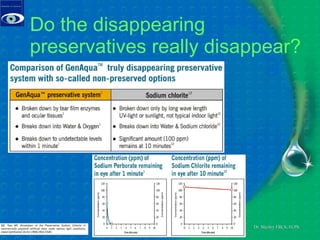
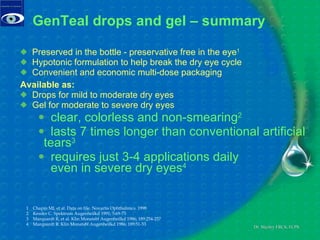
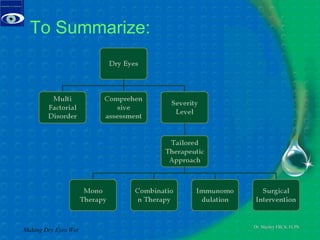
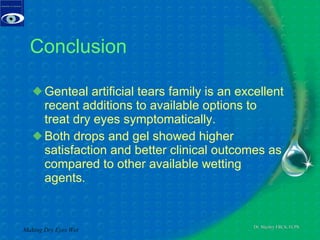
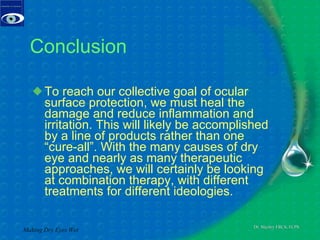
The document discusses the diagnosis and treatment of dry eye syndrome, highlighting its prevalence, symptoms, and underlying causes. Treatment approaches include patient education, environmental modifications, and various therapeutic options like artificial tears, gels, and punctal plugs. Genteal artificial tears are presented as an effective, preservative-free solution that offers significant patient satisfaction and clinical outcomes for dry eye relief.