Dry eye
- 1. 274 INTRODUCTION Dry eye syndrome (DES) is characterized by ocular irritation and visual disturbance resulting from alterations of the tear film and ocular surface.1–10 The effects of DES can vary from minor inconvenience to rare sight-threatening complications. Although the diagnosis of DES has traditionally focused on inadequate secretion or aqueous tear defi- ciency, the tear film is a complex and delicately balanced unit depend- ent on the normal function of several distinct components.10–13 Current treatment is heavily weighted toward supplementation, stimulation, or preservation of aqueous tears, which is satisfactory for many patients. DES, however, often involves multiple deficiency states that, when disregarded, can result in treatment failure and frustration for both the patient and the physician. Currently, a large unmet need exists for bet- ter treatment options for patients with DES. EPIDEMIOLOGY Estimating the prevalence of dry eye syndrome is complicated by the absence of consensus on a single reliable diagnostic test. Several population-based epidemiologic studies have utilized questionnaires to assess prevalence of dry eye symptoms. American and Australian stud- ies have revealed a prevalence of 5–16%, while Asian studies have revealed a higher prevalence of approximately 27–33%.14–25 PATHOGENESIS Normal Physiology The stratified tear film is composed of mucin, aqueous, and lipid com- ponents. The mucin layer consists of high-molecular-weight glycopro- teins closely adherent to an inherently hydrophobic surface epithelium and its glycocalyx. Mucin provides a smooth, hydrophilic surface per- mitting even distribution of the overlying aqueous layer. Its primary source is conjunctival goblet cells with a small contribution from sur- face epithelial cells.26,27 Comprising the largest volume of the tear film, the aqueous is secreted by the main lacrimal gland, the accessory glands of Krause and Wolfring, and, minimally, a transudate of the conjunctival vessels and cornea. Consisting primarily of water, it also contains electrolytes (Na, K, Cl) and proteins, including epidermal growth factor, immunoglobulins (IgA, IgG, IgM), lactoferrin, lysozyme, and other cytokines.28,29 These components likely play both a protective and a homeostatic role for the ocular surface. Lastly, meibomian glands secrete a lipid layer, containing chiefly sterol esters and wax monoesters.3,30 Although only 0.1 μm thick, the lipid layer serves to stabilize the tear film by increasing surface tension and retarding evaporation. The tear layer maintains a smooth surface for optical clarity, lubri- cates to facilitate eyelid blink, and offers protection against ocular infec- tion.11 Average tear flow is about 1.2 μm/minute.31 Blinking serves to periodically distribute tears evenly over the ocular surface and encour- ages both secretion and mechanical drainage of tears through the lac- rimal drainage system. Regulation likely involves both neuronal and hormonal pathways. Direct innervation of the lacrimal gland, meibo- mian glands, and goblet cells has been demonstrated, with M3 class cholinergic receptors predominating in the lacrimal gland.32 While estrogen has little effect on tear secretion, it may have a supportive role on the ocular surface.33 Androgens appear to have a positive effect on the secretion of both aqueous and lipid tears.34,35 Pathophysiology Reduced aqueous tear flow and increased evaporation of the aqueous component of tears leads to hyperosmolarity. Tear hyperosmolarity damages the ocular surface epithelium and sets off a cascade of inflam- matory pathways which leads to apoptotic cell death, loss of goblet cells, and deficient mucus production, with resultant tear film instabil- ity. Tear film instability, in turn, leads to increased evaporation. Impli- cated cytokines include MAP kinases, NFκB, IL-1, TNF-α, and matrix metalloproteinases (MMP-9 in particular).36–38 In the early stages of dry eye, inflammation and mechanical irritation stimulates reflex secretion from the lacrimal gland and increased blink rate. Over time, damage to the ocular surface leads to reduction in corneal sensation and impaired reflex tearing.10 In advanced cases, chronic conjunctival damage can lead to metaplasia and keratinization. Diagnosis and Classification The 2007 report from the International Dry Eye WorkShop (DEWS) defined dry eye syndrome as follows: Dry eye is a multifactorial disease of the tears and ocular surface that results in ocular discomfort, visual disturbance, and tear film instability with potential damage to the ocu- lar surface.10 This definition encompasses all the clinical entities asso- ciated with systemic disease, as well as idiopathic dry eye disease. As a result of these workshops, a classification system algorithm for dry eye was produced (Fig. 4-23-1). The effect of the environment on an indi- vidual’s risk of developing dry eye also is considered. Low blink rate,39,40 wide lid aperture,41–-43 aging,44–46 low androgen levels,47,48 high estrogen levels,49,50 and systemic drugs affect the so-called ‘milieu interieur.’10 Low relative humidity, air conditioning, air travel,51 high wind velocity, and other occupational environmental factors such as video display terminal use52 affect the so-called ‘milieu exterieur.’10 Aqueous Tear-Deficient Dry Eye Sjögren described keratoconjunctivitis sicca (KCS) in 1933.53 Conse- quently, defective lacrimal tear secretion is subdivided into non-Sjö- gren’s tear deficiency (NSTD) and Sjögren’s syndrome tear deficiency (SSTD). NSTD has no association with systemic autoimmune disease, which is a cardinal feature of SSTD. Naveen K. Rao, Michael H. Goldstein, Elmer Y. Tu 4.23Dry Eye SECTION 6 Corneal Diseases PART 4 CORNEA AND OCULAR SURFACE DISEASES Associated features ■ Possible autoimmune disease (i.e. Sjögren’s syndrome) ■ Possible conjunctival or lid abnormalities ■ Blurred or unstable vision Key features ■ Symptoms: ocular and conjunctival irritation ■ Ocular surface disruption Definition: A clinical condition characterized by deficient tear production and/or excessive tear evaporation.
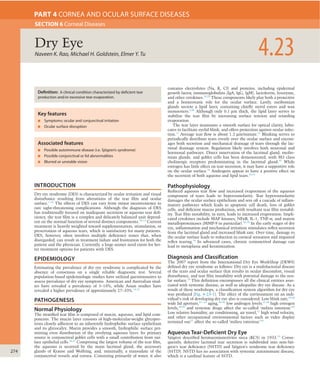
- 2. DryEye 4.23 275 common source for the inhibition of efferent lacrimal gland stimula- tion through anticholinergic activity or decreased secretion through systemic dehydration (Table 4-23-1).79 While DES has been reported in association with menopause, estrogen supplementation has not been shown to have a beneficial effect.49,80 Alterations in other hormones, especially androgens, which also are reduced during menopause, have been implicated. Sjögren’s syndrome tear deficiency Sjögren’s syndrome is a clinical condition of aqueous tear deficiency combined with dry mouth. The syndrome is classified as primary Non-Sjögren’s tear deficiency NSTD can occur from primary lacrimal gland deficiencies, secondary lacrimal gland deficiencies, obstruction of lacrimal gland ducts, or reflex hyposecretion.10 Primary lacrimal gland deficiencies include age- related dry eye, congenital alacrima, and familial dysautonomia (Riley– Day syndrome). The most common form of NSTD is age-related dry eye, which is associated with ductal and interacinar fibrosis and obstruction within the lacrimal gland, possibly as a result of low-grade chronic inflammation.54–56 Congenital alacrima is a rare cause of dry eye in youth, resulting from primarily absent or hypoplastic lacrimal glands. Familial dysautonomia is an autosomal recessive multisystem disorder in which generalized pain insensitivity accompanies absence of both emotional and reflex tearing. Defective sympathetic and para- sympathetic innervation of the lacrimal gland and defective sensory innervation of the ocular surface occur.10 Secondary lacrimal gland deficiency from infiltration and damage to the lacrimal gland in benign lymphoepithelial lesion (Mikulicz’s dis- ease), lymphoma, sarcoidosis, hemochromatosis, amyloidosis, HIV/ AIDS, and graft-versus-host disease all can result in dry eye.57–59 Surgi- cal or radiation-induced destruction or denervation of lacrimal tissue can result in secondary lacrimal deficiency.57 Secondary obstruction of the lacrimal gland ducts can occur with trachoma,60 ocular cicatricial pemphigoid, mucous membrane pemphigoid,61–63 erythema multiforme/ Stevens–Johnson syndrome,64 chemical burns, and thermal burns.65 Reflex hyposecretion of tears can be conceptually divided into reflex sensory block (damage to the afferent arm) and reflex motor block (damage to the efferent, or secretomotor arm). Reflex sensory block occurs with any reduction in ocular surface sensation and leads to decreased reflex-induced lacrimal secretion and decreased blink rate, which increases tear evaporation.10,66 Causes of decreased ocular surface sensation leading to dry eye include topical anesthetic use,67 contact lens wear,68,69 diabetes mellitus,17,70–73 aging, and neurotrophic keratitis. As shown by studies utilizing topical anesthesia, interruption of the afferent stimulus of tear production, or sensory loss (denervation), results in decreased tear secretion and reduced blink rate.67,74 Damage to afferent sensory fibers occurs after incisional corneal surgery (pene- trating or anterior lamellar keratoplasty, radial keratotomy, and limbal cataract incision) and after damage to the first division of the trigemi- nal ganglion from trauma, tumor, herpes simplex, or zoster, resulting in reduced tear production. LASIK and photorefractive keratectomy result- ing in decreased corneal sensation and blink rate are recognized as precipitating causes of dry eye.66,75–77,78 Systemic medications are a Fig. 4-23-1 Dry eye classification. (With permission from Lemp MA.The 1998 Castroviejo Lecture. New strategies in the treatment of dry-eye states. Cornea 1999;18:625–32.) Contact lens Rheumatoid arthritis Systemic lupus erythematosus Wegener's granulomatosis Systemic sclerosis Primary biliary cirrhosis Other autoimmune diseases primary secondary Sarcoid HIV Graft vs. host Xerophthalmia ablation Other diseases Posterior blepharitis Obstructive meibomian gland disease Anterior blepharitis Sjögren's syndrome Non-Sjögren tear deficiency Lacrimal obstruction Reflex Oil deficient Lid related Surface changeLacrimal disease Trachoma, cicatricial pemphigoid Erythema multiforme Burns Neuro-paralytic keratitis Contact lens VIIth nerve palsy Absent glands Distichiasis Blink abnormalities Aperture abnormalities Lid surface incongruity Xerophthalmia Congenital alacrima acquired primary lacrimal gland disease Tear deficient EvaporativeDry eye – keratoconjunctivitis sicca DRY EYE CLASSIFICATION TABLE 4-23-1 MEDICATIONS ASSOCIATED WITH DRY EYE SYNDROME Mechanism of Action Class Medications Anticholinergic Antimuscarinics Tolterodine tartrate (Detrol) Scopolamine Antihistamines (sedating compounds are associated with greater dryness) Chlorpheniramine (Chlor- Trimeton) Diphenhydramine (Benadryl) Promethazine (Phenergan) Anti-parkinsonian Benzotropine (Cogentin) Trihexyphenidyl (Artane) Antidepressants MAO inhibitors Amitriptyline (Elavil) Nortriptyline (Pamelor) Imipramines (Tofranil) Doxepin (Sinequan) Phenelzine Antipsychotics Chlorpromazine (Thorazine) Thioridazine (Mellaril) Fluphenazine (Prolixin) Antimanics Lithium Antiarrhythmics Disopyramide (Norpace) Mexiletine (Mexitil) Antiadrenergic Alpha-agonists Clonidine (Catapres) Methyldopa (Aldomet) Beta-blockers Propranolol (Inderal) Metoprolol (Lopressor) Diuretic Thiazides Hydrochlorothiazide Other NSAIDs Ibuprofen (Advil) Naproxen (Naprosyn, Aleve) Cannabinoids Marijuana
- 3. 4 276 CORNEAANDOCULARSURFACEDISEASES the meibomian gland orifices remain anterior to the mucocutaneous junction, whereas in cicatricial MGD the meibomian gland orifices are drawn posteriorly onto the lid and tarsal mucosa. Exposure Excessive exposure of the ocular surface leads to increased evaporative loss of tears; thus, any disorder that results in increased ocular expo- sure can cause evaporative dry eye. Psychological, psychiatric, mechani- cal, neurological, or traumatic impairment of eyelid function may result in impaired or reduced blinking, lagophthalmos, or an increased palpebral fissure width, resulting in an evaporative dry eye. Evaporative dry eye can be seen in thyroid eye disease secondary to proptosis or lid retraction. Mucin Deficiency Local conjunctival damage from cicatrizing disease or surgical trauma results not only in aqueous tear deficiency, but also in depopulation of mucin-producing goblet cells and creation of anatomical abnormalities of the conjunctiva leading to improper tear distribution. Although uncommon in incidence, trachoma, pemphigoid, erythema multiforme/ Stevens–Johnson syndrome, and chemical and thermal burns can result in severe DES characteristically resistant to aqueous tear replace- ment therapy. Extrinsic Causes Vitamin A deficiency can result in extensive goblet cell loss and dys- function, leading to an unstable tear film and severe dry eye (xeroph- thalmia).91–94 Preservatives in many eye drops (especially benzalkonium chloride) can lead to ocular surface toxicity and a dry eye state that may be reversible if eye drops are switched to nonpreserved formulations. Contact lens wear is commonly associated with dry eye symptoms. Pre-lens tear film thinning time and pre-lens lipid layer thickness is reduced in contact lens wearers with dry eye symptoms, and may lead to higher evaporative loss.95 Ocular allergies can cause a variety of cor- neal and conjunctival irregularities with decrease in tear film stability and consequent dry eye. OCULAR MANIFESTATIONS Regardless of the cause, most forms of dry eye share similar symptoms, interpalpebral surface damage, tear instability, and tear hyperosmolar- ity. Typical complaints include burning, itching, foreign body sensation, stinging, dryness, photophobia, ocular fatigue, and redness. Although symptoms are usually nonspecific, careful attention to details will help refine the diagnosis. Patients commonly describe a diurnal pattern with aqueous tear deficiency with progression of symptoms over the day and decompensa- tion in particular environmental conditions such as low humidity in airline cabins, climate control, and the use of video display termi- nals.52,96 Conversely, night-time exposure, floppy eyelid syndrome, and inflammatory conditions often present with worst discomfort upon awakening. Meibomian gland disease creates an unstable tear film resulting in intermittent visual blurring and a gritty or sandy sensation. DES in diabetes and other corneal neuropathies may exhibit little or no dis- comfort and create high risk for keratolysis. Common signs of DES include conjunctival injection, decreased tear meniscus, photophobia, increased tear debris, and loss of corneal sheen found more commonly in the exposed interpalpebral fissure. Paradoxi- cal epiphora in DES is usually a result of reflex tearing. Greater risk for external infections exists secondary to decreased tear turnover and desiccation of the surface epithelium. Instability of the surface epithelium and disordered mucin production may lead to painful and recurrent filamentary keratitis. Although keratinization may occur uncommonly in chronic DES, vitamin A deficiency also should be suspected. Patients who have SSTD tend to have more severe symptoms and more serious findings than do NSTD patients. Sterile ulceration of the cornea in SSTD can be peripheral or paracentral; both thinning and perforation of these ulcers can occur (Fig. 4-23-2). Acute lacrimal enlargement may be seen in SSTD but should be differentiated from benign lymphoepithelial lesion (Mikulicz’s disease), which results from infiltration of the gland without surface findings.97 (patients without a defined connective tissue disease) or secondary (patients who have a confirmed connective tissue disease).81,82 Primary SSTD refers to aqueous tear deficiency combined with symptoms of dry mouth, presence of autoantibodies to Ro(SSA) or La(SSB) antigens, decreased salivary secretion, and presence of lymphocytic foci on minor salivary gland biopsy. Secondary SSTD is associated with rheumatoid arthritis, systemic lupus erythematosus, polyarteritis nodosa, Wegen- er’s granulomatosis, systemic sclerosis, primary biliary cirrhosis, and mixed connective tissue disease.10,82 Both subtypes of SSTD feature progressive lymphocytic infiltration of the lacrimal and salivary glands and can be associated with severe and painful ocular and oral discom- fort. The pathogenesis of the tear deficit in SSTD is infiltration of the lacrimal gland by B and CD4 lymphocytes (with some CD8 lym- phocytes) and by plasma cells, with subsequent fibrosis. Revised American-European consensus diagnostic and classification criteria for Sjögren’s syndrome were published in 2002.82 One point is given for at least one positive response or positive result in each of the following categories: •Ocular symptoms: daily dry eye symptoms for more than 3 months, ocular irritation, use of artificial tears more than 3 times per day •Oral symptoms: daily dry mouth symptoms for more than 3 months, presence of swollen salivary glands, frequent drinking of liquids to aid in swallowing •Ocular signs: Schirmer I test (without anesthetic) ≤ 5 mm in 5 min- utes, rose bengal score ≥4 according to the van Bijsterveld scoring system •Histopathology: biopsy of minor salivary gland showing inflamma- tion with lymphocytic foci •Oral signs: reduced salivary flow ≤1.5 ml in 5 minutes, parotid sialography showing salivary duct dilation without obstruction, salivary scintigraphy showing signs of decreased saliva production •Autoantibodies: presence of anti-Ro(SSA) antibody, presence of anti-La(SSB) antibody. For a diagnosis of primary Sjögren’s syndrome, either four of the six categories (including either histopathology or autoantibodies) or three of the four objective categories (ocular signs, histopathology, oral signs, and autoantibodies) must be met. For diagnosis of secondary Sjögren’s syndrome, in patients with a defined connective tissue disease, the presence of one symptom (ocular or oral) plus two of the three objective categories (ocular signs, histopathology, and oral signs) must be met. Evaporative Dry Eye Excessive evaporation that occurs in specific periocular disorders can cause dry eye disease with or without concurrent aqueous tear defi- ciency. Evaporation leads to both loss of tear volume and a dispropor- tionate loss of water, resulting in tear hyperosmolarity. Environmental conditions such as high altitude, dryness, or extreme heat accelerate evaporative tear loss even in normal eyes. Causes of evaporative dry eye can be intrinsic (disease affecting lid structures or dynamics) or extrinsic.10 Meibomian Gland Disease and Blepharitis Meibomian gland dysfunction (MGD) leads to both decreased secretion and abnormal composition of the tear film lipid layer. The abnormal composition leads to meibomian gland blockage and reduced effective- ness in the tear film. The resulting ocular surface and eyelid inflamma- tion perpetuates a cycle of inflammation, scarring, hyperkeratosis, stenosis, and further MGD. Often associated, bacterial colonization by normal lid commensals (Staphylococcus aureus, Propionobacterium acnes, and coagulase- negative staphylococci) acts directly by altering secreted lipids and indirectly by causing inflammation. Esters and lipases produced by these commensals act on secreted lipids in the tear film, producing soaps that manifest as ‘meibomian foam.’83,84 An association is also seen with dermatologic conditions such as seborrheic dermatitis, atopic dermatitis, and acne rosacea, a disorder resulting in vascular dilation, telangiectasias, and plugging of sebaceous glands of both facial and eyelid skin. Secondary MGD can occur with use of 13-cis retinoic acid (isotretinoin) for treatment of acne,85–87 ingestion of polychlorinated biphenyls in contaminated cooking oil,88–90 and with cicatricial changes in conditions such as chemical/thermal burns, trachoma, pemphigoid, erythema multiforme/Stevens–Johnson syndrome, acne rosacea, vernal keratoconjunctivitis, and atopic keratoconjunctivitis.10 In simple MGD,
- 4. DryEye 4.23 277 diagnosis of DES, and a result of 6–10 mm of wetting suggests a dry eye problem.104 Hamano et al. developed the phenol red thread test to obviate the disadvantages of Schirmer’s test by eliminating the need for anesthe- sia.105 Three millimeters of a fine dye-impregnated 75 mm cotton thread is placed under the lateral one-fifth of the inferior palpebral lid margin for 15 seconds; alkalinity changes its color to bright orange from tear contact. Asian populations show a lessened wet-length response with diminishing racial differences with advancing age.106 Hyperosmolarity is a common endpoint for all DES. Its measure- ment can be a sensitive and specific indicator.104 Its use has been lim- ited to specialized research centers due to the need for expensive equipment, but new commercially available devices may make this test more widely used in the future. Other rarely performed tests for reduced tear function include fluorophotometry for decreased protein content, lysozyme levels, ocular ferning, impression cytology, and lactoferrin assays. Noninvasive imaging of the tear film using menis- cometry, lipid layer interferometry, high-speed videography, optical coherence tomography, and confocal microscopy has been advocated as well.107–111 Other Tests Corneal sensation may be qualitatively assessed with a cotton wisp, but quantification requires an instrument such as the Cochet–Bonnet aes- thesiometer. The tear clearance test measures tear turnover with serial tear collection after instillation of a standardized volume of dye.103,112 Serological tests, including antinuclear, anti-Ro, and anti-La antibodies, should be performed in patients suspected of having autoimmune DES. A definitive diagnosis of Sjögren’s syndrome requires minor salivary or, rarely, lacrimal gland biopsy. Neither clinical presentation nor individ- ual ancillary tests alone are sufficient for an accurate diagnosis of DES. Because of the therapeutic importance of appropriate categorization of patients, Pflugfelder et al. combined standard subjective examination with ancillary tests in the evaluation of SSTD, NSTD, inflammatory MGD, and atrophic MGD patients.113 Clinically important results were identified and compiled into an algorithm that helps differentiate DES patients with available tests (Fig. 4-23-4). TREATMENT Significant advances have been made in treating the many facets of dry eye, but it remains a disorder of long-term maintenance rather than permanent cure. Current therapy focuses on restoring a normal ocular surface through tear supplementation as well as inhibition of aberrant inflammation seen in chronic DES. Since the tear film is a highly inte- grated unit, addressing each component is central to the successful treatment of DES. Aqueous Tear Deficiency As the first line of treatment, artificial tears increase available tears and, through dilution, reduce tear hyperosmolarity. Commercial artifi- cial tears differ in electrolyte composition, thickening agents (methyl- cellulose, hydroxypropyl methylcellulose, polyvinyl alcohol), physiologic buffering, tonicity, and preservative system. Individual patient prefer- ences involve such disparate concerns as cost, comfort, visual blurring, and ease of use. Preserved tears (i.e. benzalkonium chloride) can be toxic in moderate or severe dry eye, are poorly tolerated, and harmful. For patients with significant dry eye, single-dose, nonpreserved tear preparations are the mainstay of therapy with bottled tear products a reasonable alternative when preserved with relatively nontoxic compounds. These less toxic preservatives include polyquaternium-1, sodium chlorite, and sodium perborate.114 Some artificial tear prepara- tions are formulated to be hypo-osmotic, with the goal of balancing the hyperosmolarity of the tear film in dry eye. Artificial tear ointments are effective for longer-lasting control of symptoms, especially during sleep, but visual blurring limits their daytime usefulness. In addition, some ointments contain lanolin and parabens, which can be poorly tolerated by patients with severe dry eye. Autologous serum tears contain trophic factors and other proteins useful in ocular surface maintenance.114 These can be useful as a preservative-free, biological tear substitute, but their preparation is labor-intensive. Punctal occlusion retards tear drainage, thereby increasing tear vol- ume on the ocular surface and lowering tear osmolarity. Occlusion may be achieved irreversibly by cauterization or semi-permanently with the DIAGNOSIS AND ANCILLARY TESTING Diagnostic Dye Evaluation Fluorescein is a large molecule unable to traverse normal corneal epi- thelial tight junctions. In advanced DES, these junctions are disrupted, allowing characteristic diffuse subepithelial or punctate staining. Rose bengal, a derivative of fluorescein, in a 1% solution or impregnated strips, stains devitalized epithelial cells (Fig. 4-23-3).98 Alternatively, lissamine green stains for cell death or degeneration, as well as cell-to- cell junction disruption, but does not irritate the eye.99 Tear Film Stability Tear film instability may be a result of either tear deficiency or evapora- tive DES. In the tear breakup time (TBUT) test, described by Norn and revised by Lemp and Holly, fluorescein dye is instilled and the time interval is measured between a complete blink to the first appearance of a dry spot in the precorneal tear film.100 TBUTs shorter than 10 seconds indicate tear film instability. Measurement of Tear Production The most common means of measuring tear production has been Schirmer’s test, the details of which were first published in 1903.101 Jones later advocated the use of topical anesthesia combined with a Schirmer’s test strip for 5 minutes to reduce the stimulating effect of the filter paper strip – the ‘basal’ tear secretion test.102 Inconsistencies in its application limit repeatability in DES, but it still enjoys wide- spread use.103 With these caveats in mind, the following general guide- lines are recommended (when topical anesthesia is used): a 5-minute test that results in less than 5 mm of wetting confirms the clinical Fig. 4-23-2 Patient age 73 with rheumatoid arthritis and secondary Sjögren’s syndrome. Fig. 4-23-3 Dry eye syndrome with rose bengal staining.
- 5. 4 278 CORNEAANDOCULARSURFACEDISEASES the ocular surface by tear supplementation alone. DES-induced ocular surface inflammation disrupts the epithelial and mucin layers, further exacerbating tear film breakdown. Suppression of inflammation creates a supportive environment for reversal of DES-induced cellular chang- es.118,119 Topical cyclosporine A has been shown to increase tear produc- tion in a subset of patients through inhibition of lacrimal gland inflammation and suppression of DES-induced ocular surface inflammation.120–122 Judicious use of low-dose topical corticosteroids has been shown to reduce inflammation and allow normal reparative mechanisms to restore the natural equilibrium of the ocular sur- face.123,124 Control of these reactive epithelial changes restores normal cell morphology, cell-to-cell interactions, and critical mucin production and clearly has a role in the global treatment of all forms of DES. Essential fatty acids cannot be synthesized by humans and must be consumed in the diet. The typical Western diet contains a ratio of omega-6 to omega-3 fatty acids of approximately 25 to 1.114 Omega-6 fatty acids are precursors to arachidonic acid and proinflammatory molecules, including PGE2 and LTB4. Omega-3 fatty acids inhibit syn- thesis of these inflammatory mediators and decrease production of IL-1 and TNF-α.125,126 Supplementing the diet with omega-3 fatty acids has been shown to decrease both signs and symptoms of dry eye.127 Omega- 3 fatty acids include eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). EPA and DHA are believed to be primarily responsible for the beneficial health effects of omega-3 fatty acids. Fish oil contains high levels of EPA and DHA, and flaxseed oil contains high levels of ALA. While ALA is converted by the body into EPA and DHA, this process is not efficient, so much higher quanti- ties of flaxseed oil must be consumed to achieve equivalent EPA and DHA levels from smaller quantities of fish oil.128,129 A number of drugs (mostly topical and a few systemic) are currently being evaluated in clinical trials aimed at providing new treatment options for patients with DES.130,131 Success with this research should provide patients with many more treatment options in the future and has the potential to improve quality of life for patients suffering with DES.132 KEY REFERENCES The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). The Ocular Surface 2007;5: 75–92. The Epidemiology of Dry Eye Disease: Report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). The Ocular Surface 2007;5:93–107. Ang RT, Dartt DA, Tsubota K. Dry eye after refractive surgery. Curr Opin Ophthalmol 2001;12: 318–22. use of nonabsorbable plugs. Occlusion with collagen plugs provides temporary relief (3 days to 6 months) and may identify those at risk for epiphora prior to permanent occlusion. Epiphora in the setting of one functional punctum is uncommon. Secretagogues, agents that stimulate lacrimal gland secretion, require functional glandular tissue. Oral pilocarpine (Salagen) and cevimeline (Evoxac) are M3 cholinergic agonists approved for use in dry mouth that also stimulate tear secretion.32,115,116 Their effect tends to be greater in oral rather than ocular dryness. Systemic cholinergic side- effects such as sweating reduce patients’ acceptance. Various nutri- tional supplements are also touted for DES but without clear confirmation of their efficacy. Evaporative Dry Eye Primary treatment of MGD involves improving the quality and quan- tity of native meibomian gland secretions. Lid hygiene, in the form of warm compresses and lid massage, is effective in improving meibomian gland secretion. Lid scrubs with dilute detergents decrease the sebor- rheic or bacterial load, thereby breaking the proinflammatory cycle of MGD. Systemic tetracyclines have been shown to decrease local inflammation and improve meibomian gland function after several weeks. The antibacterial effect also contributes to a decrease in meibo- mian lipid breakdown products in the tear film. Topical erythromycin or azithromycin applied to the eyelid margins are alternatives for patients who are unable to tolerate tetracycline derivatives. A number of lipid-like tear substitutes have become commercially available, which have been used with some success.117 Correction of eyelid abnormalities that increase exposure of the ocular surface, such as lower lid ptosis and lagophthalmos, can stabilize a decompensated ocular surface. In severe cases, a partial or complete tarsorrhaphy or a conjunctival flap may be necessary to prevent decom- pensation of the cornea. The use of humidifiers, moisture chambers, glasses, or goggles increases periocular humidity and decreases surface evaporative pressure. New high-Dk (oxygen permeability), high-water- content contact lenses and new polymer lenses, accompanied by proper tear supplementation and hygiene, are effective in treating DES patients with poor corneal wetting. In patients with severe dry eye, scleral contact lenses can promote lubrication and slow evaporation of tears from the ocular surface. Ocular Surface Inflammation Ocular surface inflammation and its consequential cellular changes are not only a common endpoint of all DES, but also prevent restoration of Fig. 4-23-4 Diagnostic algorithm for ocular irritation. (With permission from Pflugfelder SC,Tseng SC, Sanabria O, et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea 1998;17:38–56.) No Yes Consider nontear film related problems Fluorescein tear break-up time 10 sec 1. Schirmer 1 5 mm in one or both eyes 2. Aqueous tear deficiency pattern on fluorescein clearance test 3. Grid distortion by xeroscope Symptoms of ocular irritation Tear film instability Yes Meibomian gland disease NoYes Yes No Meibomian gland pathologic signs 1. Orifice metaplasia 2. Acinar atrophy 3. Reduced expressible meibum Aqueous tear deficiency 1. Absence of nasal-lacrimal reflex 2. Presence of serum autoantibodies 3. van Bijsterveld rose bengal staining score 3 4. Exposure zone fluorescein staining score 3 Sjögren syndrome Non-Sjögren syndrome ALGORITHM FOR OCULAR IRRITATION
- 6. DryEye 4.23 279 Solomon A, Dursun D, Liu Z, et al. Pro- and anti-inflammatory forms of interleukin-1 in the tear fluid and conjunctiva of patients with dry-eye disease. Invest Ophthalmol Vis Sci 2001;42:2283–92. Stern ME, Gao J, Siemasko KF, et al. The role of the lacrimal functional unit in the pathophysiology of dry eye. Exp Eye Res 2004;78:409–16. Sullivan DA, Hammitt KM, Schaumberg DA, et al. Report of the TFOS/ARVO Symposium on global treatments for dry eye disease: an unmet need. Ocul Surf 2012;10:108–16. Tseng SC, Tsubota K. Important concepts for treating ocular surface and tear disorders. Am J Ophthalmol 1997;124:825–35. Vitali C, Bombardieri S, Jonnson R, et al. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 2002;1:554–8. Wilson SE. Laser in situ keratomileusis-induced (presumed) neurotrophic epitheliopathy. Ophthalmology 2001;108:1082–7. Barabino S, Chen Y, Chauhan S, et al. Ocular surface immunity: homeostatic mechanisms and their disruption in dry eye disease. Prog Retin Eye Res 2012;31:271–85. Begley CG, Chalmers RL, Abetz L, et al. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity. Invest Ophthalmol Vis Sci 2003;44:4753–61. Fox RI, Michelson P. Approaches to the treatment of Sjögren’s syndrome. J Rheumatol Suppl 2000;61:15–21. Lemp MA. The 1998 Castroviejo Lecture New strategies in the treatment of dry-eye states. Cornea 1999;18:625–32. Rolando M, Zierhut M. The ocular surface and tear film and their dysfunction in dry eye disease. Surv Ophthalmol 2001;45(Suppl 2):S203–10. Schaumberg DA Sullivan DA, Buring JE, et al. Prevalence of dry eye syndrome among US women. Am J Ophthalmol 2003;136:318–26. Schein OD, Hochberg MC, Munoz B, et al. Dry eye and dry mouth in the elderly: a population- based assessment. Arch Intern Med 1999;159:1359–63. Schein OD, Munoz B, Tielsch JM, et al. Prevalence of dry eye among the elderly. Am J Ophthalmol 1997;124:723–8. Access the complete reference list online at
