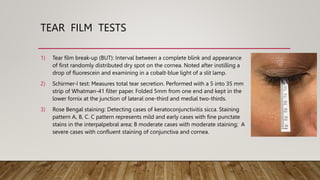
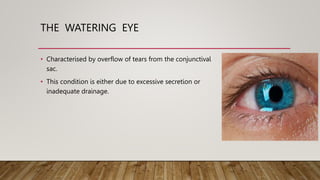
Dry eye is a multifactorial disease of the tears and ocular surface resulting in discomfort, visual disturbance, and tear film instability, with potential damage to the ocular surface. It is classified into aqueous deficiency dry eye (caused by lack of tear production) and evaporative dry eye (caused by excessive tear evaporation). Clinical features include irritation, foreign body sensation, dryness, and signs of tear film instability, conjunctival changes, and corneal signs. Complications can include vision-threatening conditions like corneal ulcer and perforation. Diagnostic tests include tear break-up time, Schirmer test, and Rose Bengal staining. Treatment focuses on tear supplementation, anti-inflammatories, secretagogues