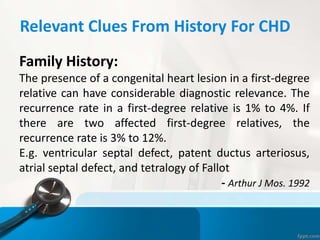
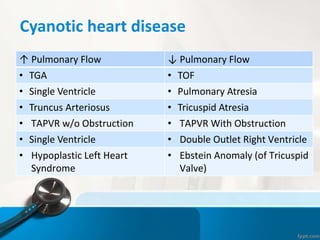
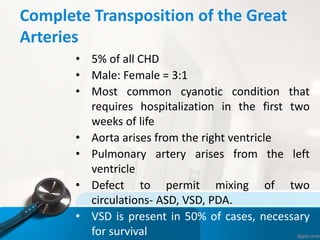
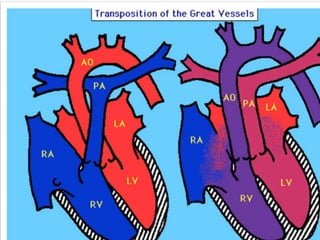
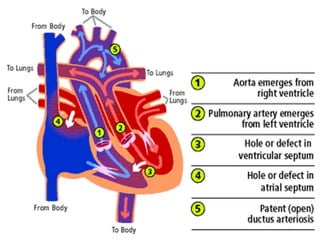
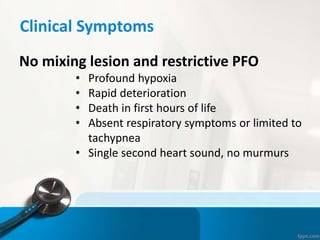
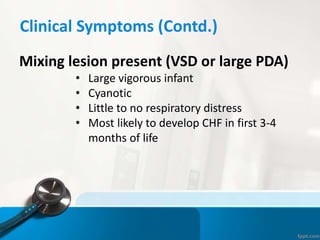
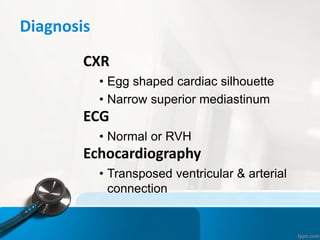
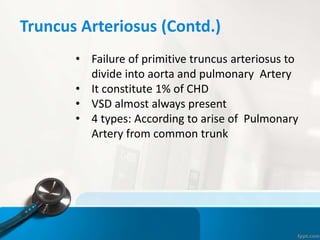
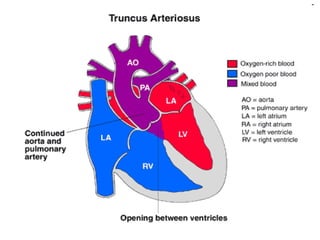
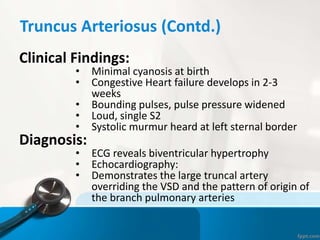
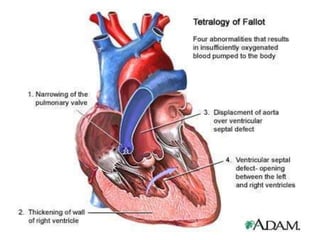
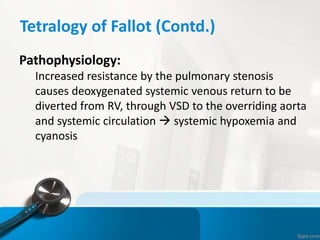
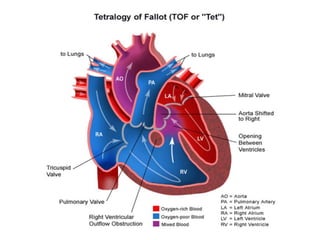
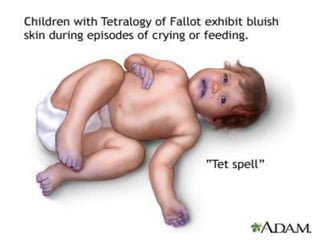
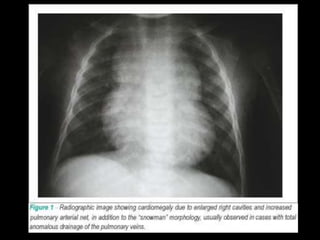
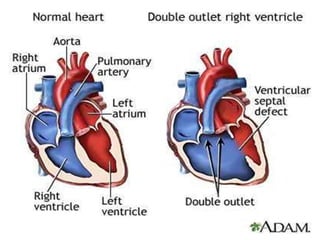
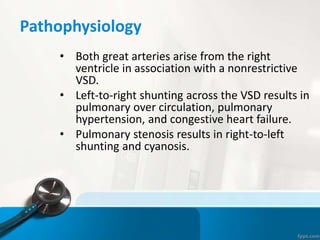
This document provides a case scenario of a 4-week-old male infant presenting with cyanosis after feeding or crying. On examination, the infant has purplish lips, hands and feet, a grade III/VI systolic murmur, and tests revealing low oxygen levels that increase slightly with oxygen. The document discusses possible diagnoses of congenital cyanotic heart disease such as tetralogy of Fallot and asks what the diagnosis could be. It then provides an overview of tetralogy of Fallot and its characteristics.