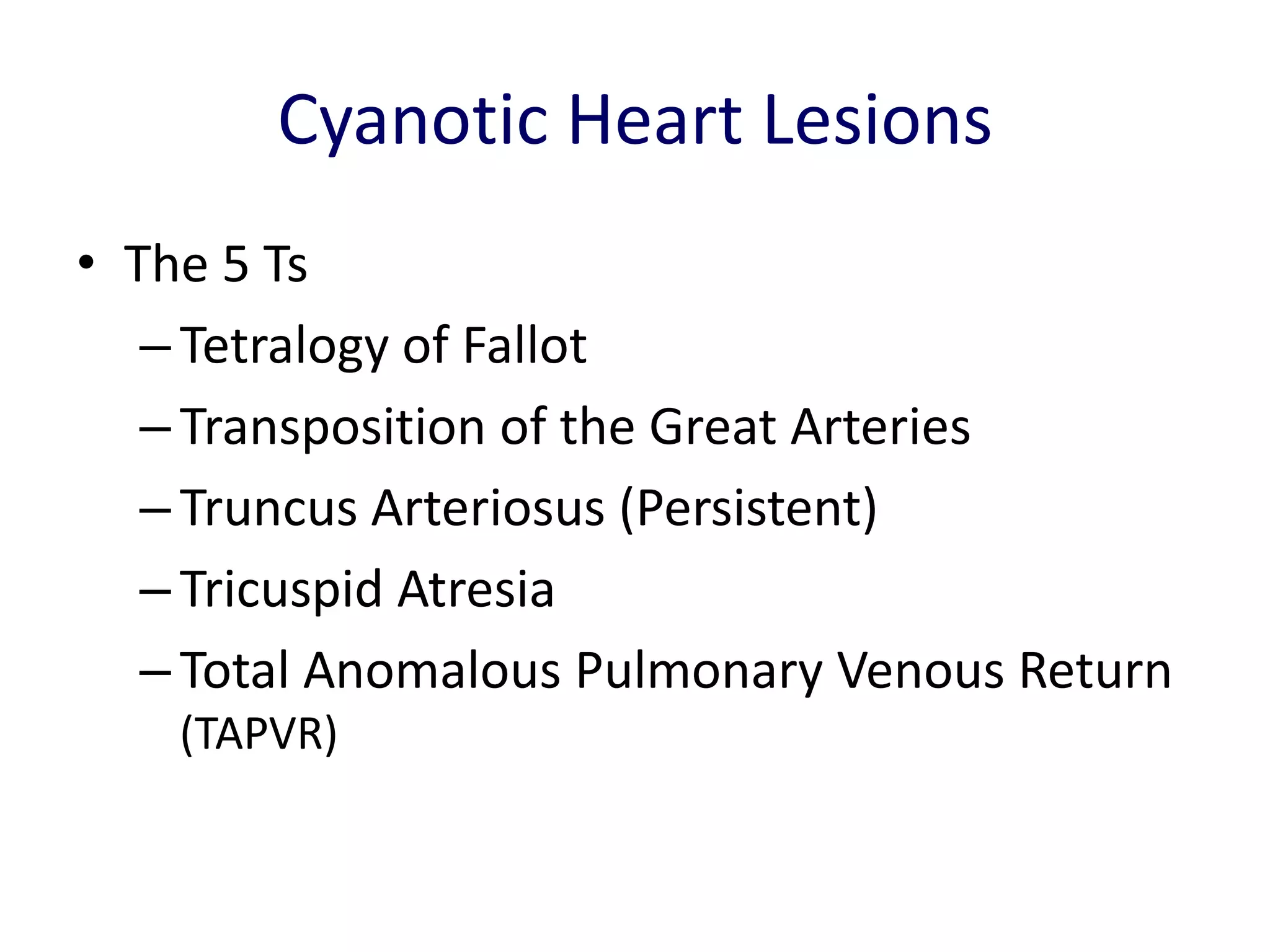
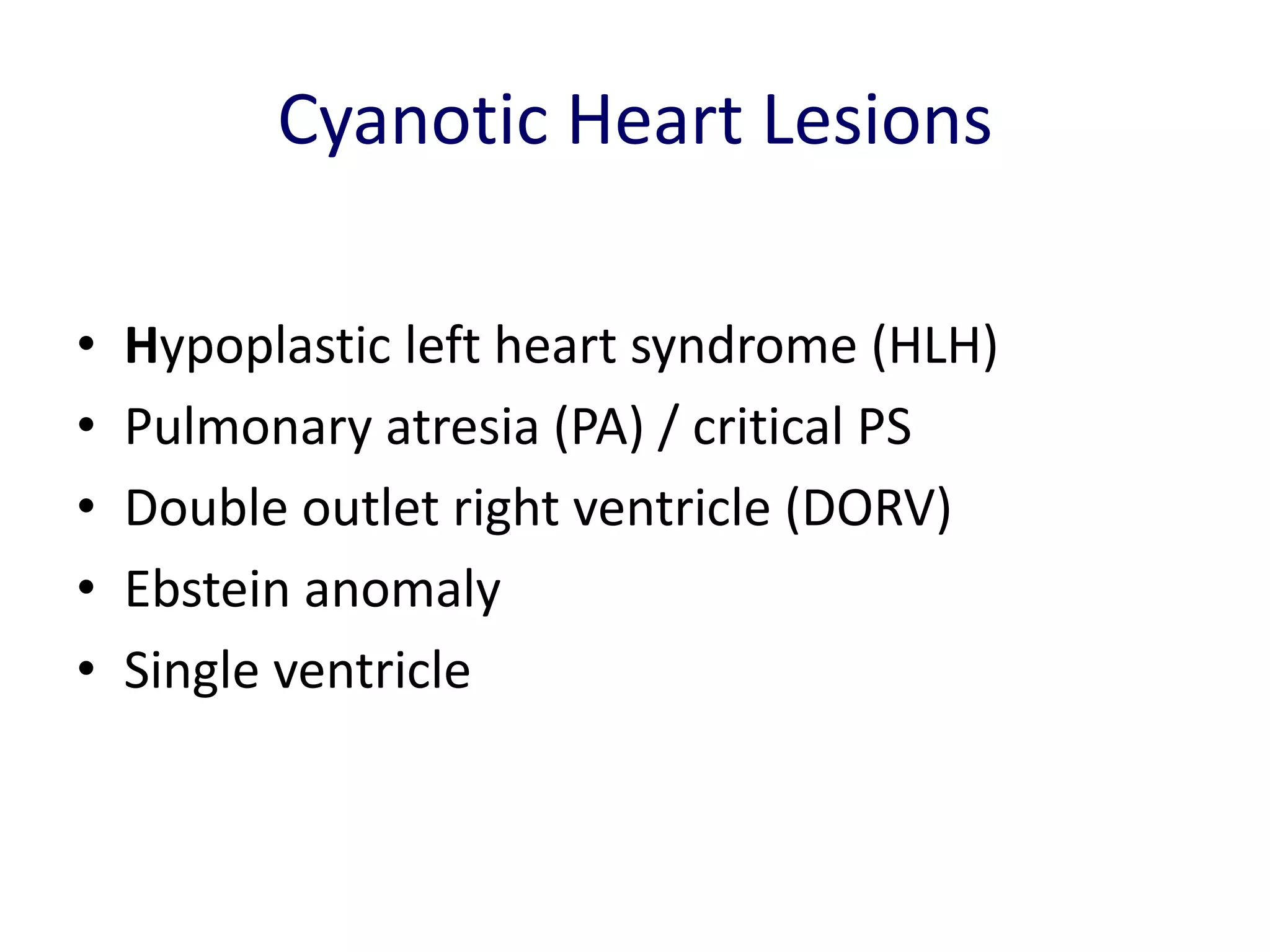
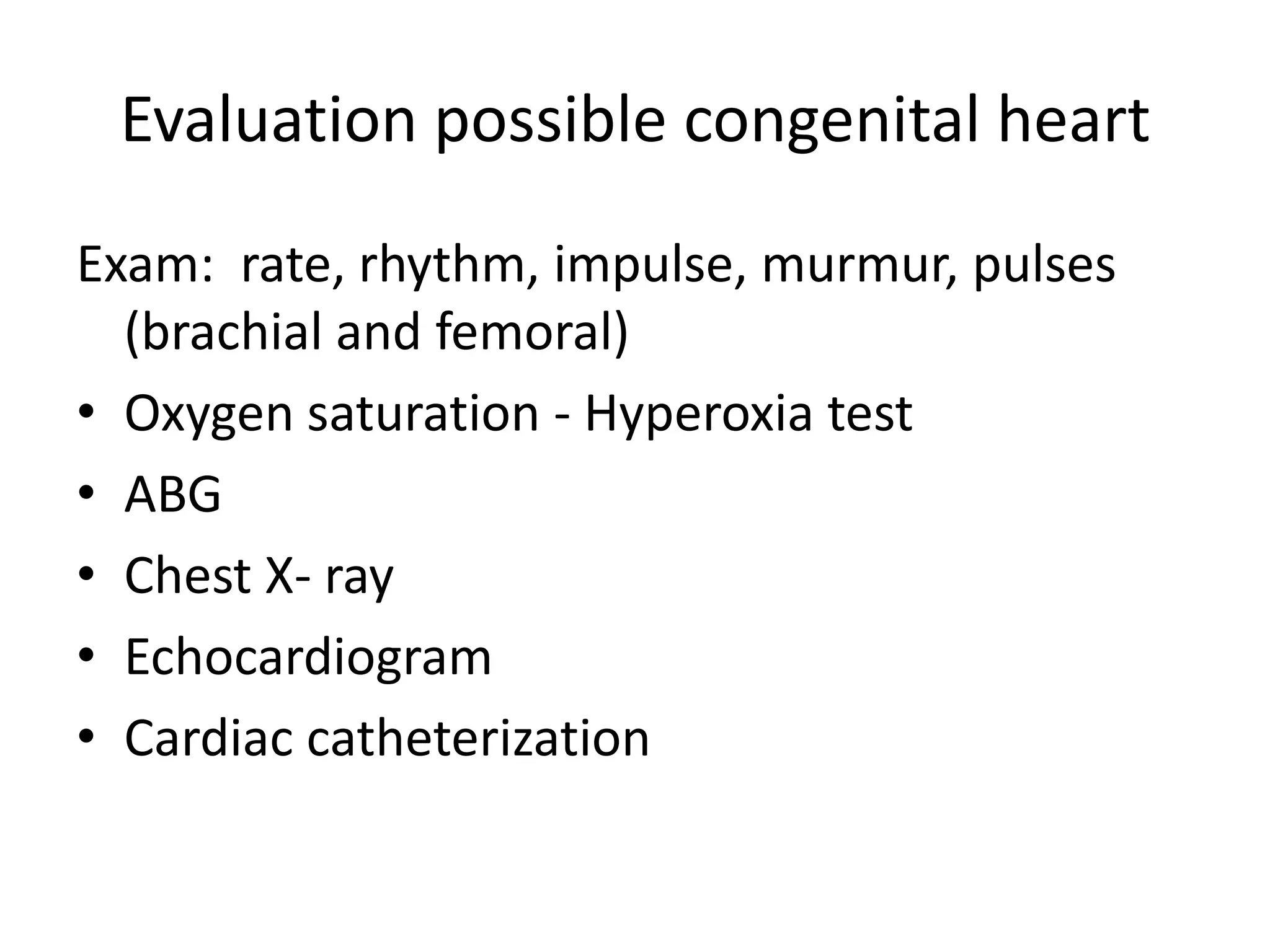
This document provides information on various cyanotic heart lesions including Tetralogy of Fallot, Transposition of the Great Arteries, Tricuspid Atresia, Ebstein's Anomaly and Total Anomalous Pulmonary Venous Return. It describes the anatomy, clinical features, diagnosis and management of these conditions. Key cyanotic heart lesions are characterized by mixing of oxygenated and deoxygenated blood resulting in central cyanosis.
![Cyanotic Heart Lesions
Dr. Kalpana Malla
MBBS MD (Pediatrics)
Manipal Teaching Hospital
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/cvs-cyanoticheartlesions-120103110643-phpapp02/75/Cyanotic-Heart-Diseases-1-2048.jpg)


![Thank you
Download more documents and slide shows on The Medical Post
[ www.themedicalpost.net ]](https://image.slidesharecdn.com/cvs-cyanoticheartlesions-120103110643-phpapp02/75/Cyanotic-Heart-Diseases-70-2048.jpg)