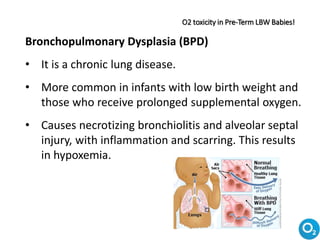
This document provides information about oxygen therapy for children. It defines oxygen and why oxygen therapy is used to treat conditions caused by low blood oxygen levels. It describes the different modes of oxygen delivery including nasal prongs, masks, and ventilators. It covers indications for oxygen therapy, sources of oxygen like cylinders, and important considerations like humidification and hazards of oxygen toxicity from high concentrations over long periods.













![FiO2 (Fraction of inspired O2) :
FiO2 is the assumed fraction (or percentage) of oxygen
concentration participating in gas exchange in the alveoli;
natural air contains 20.9% oxygen, which is equivalent to FiO2
of 0.21 or 21%. Patients given oxygen-enriched air breathe air
with a higher-than-atmospheric FiO2.
WHO, ‘Oxygen therapy for children: a manual for health workers’, 2016, p. 4.
Formula for estimation of FiO2 :
FiO2% O2 delivered = 21% + [(nasal cannula flow (L/min) x 3)]](https://image.slidesharecdn.com/oxygentherapy-171004150412/85/Oxygen-therapy-14-320.jpg)