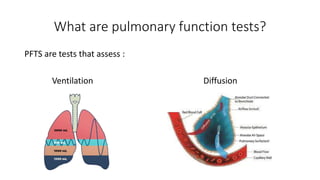
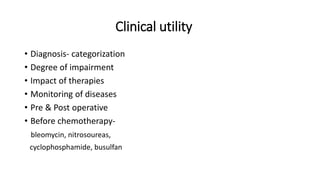
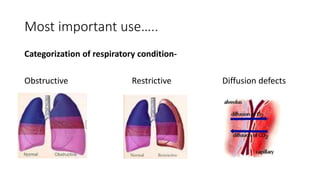
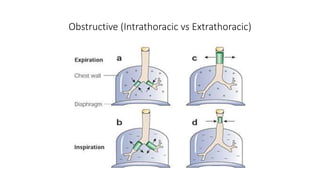
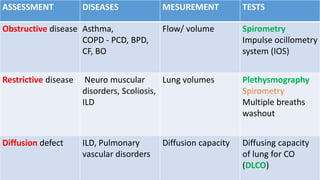
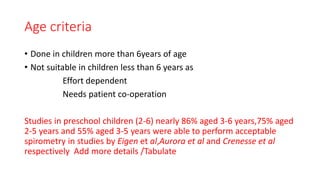
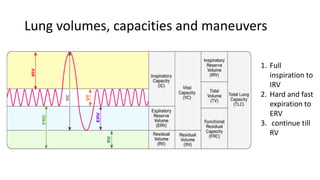
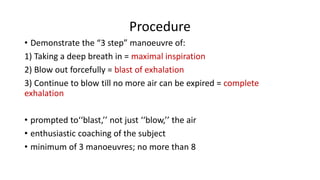
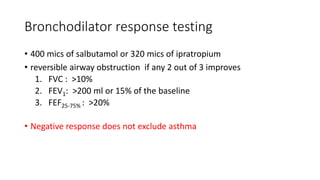
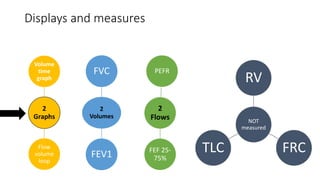
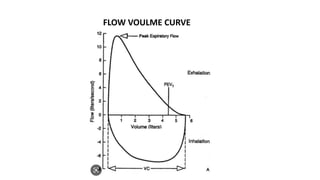
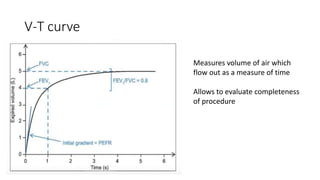
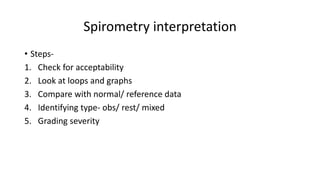
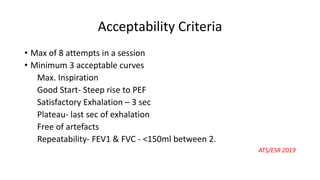
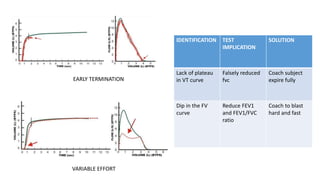
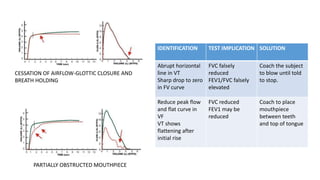
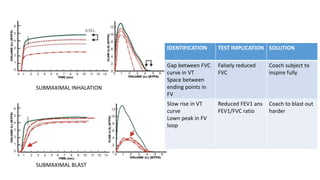
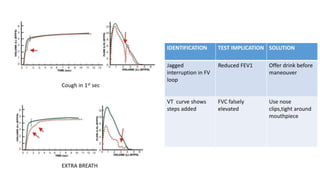
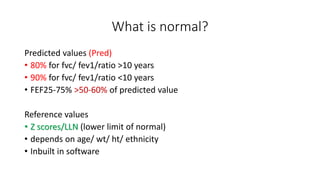
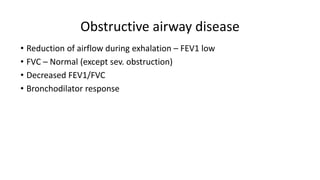
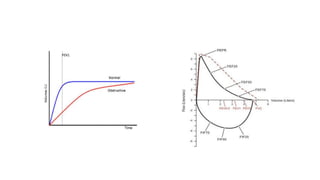
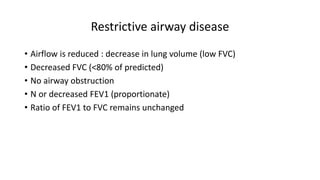
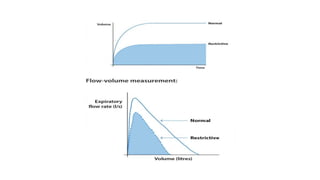
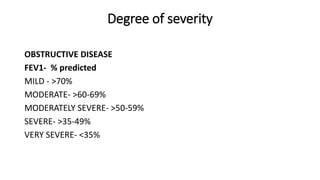
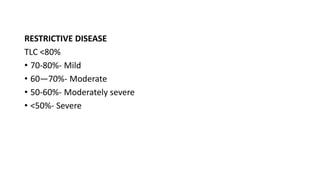
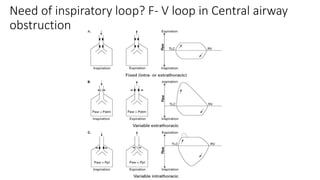
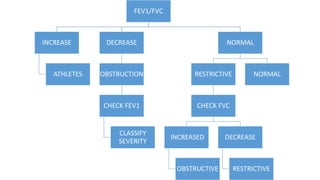
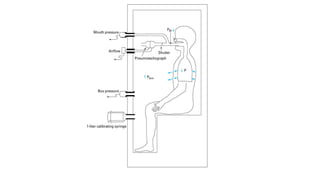
Pulmonary function tests (PFTs) are used to assess lung function in infants and children. The main types of PFTs include spirometry, plethysmography, and gas dilution techniques. Spirometry is the gold standard test for diagnosing obstructive lung diseases like asthma. It measures airflow and lung volumes. PFTs can help diagnose and categorize restrictive and obstructive lung conditions. While useful, PFTs remain underutilized in pediatrics due to challenges with availability, expertise, and limited reference data in children. Proper technique and effort are important for accurate PFT results.