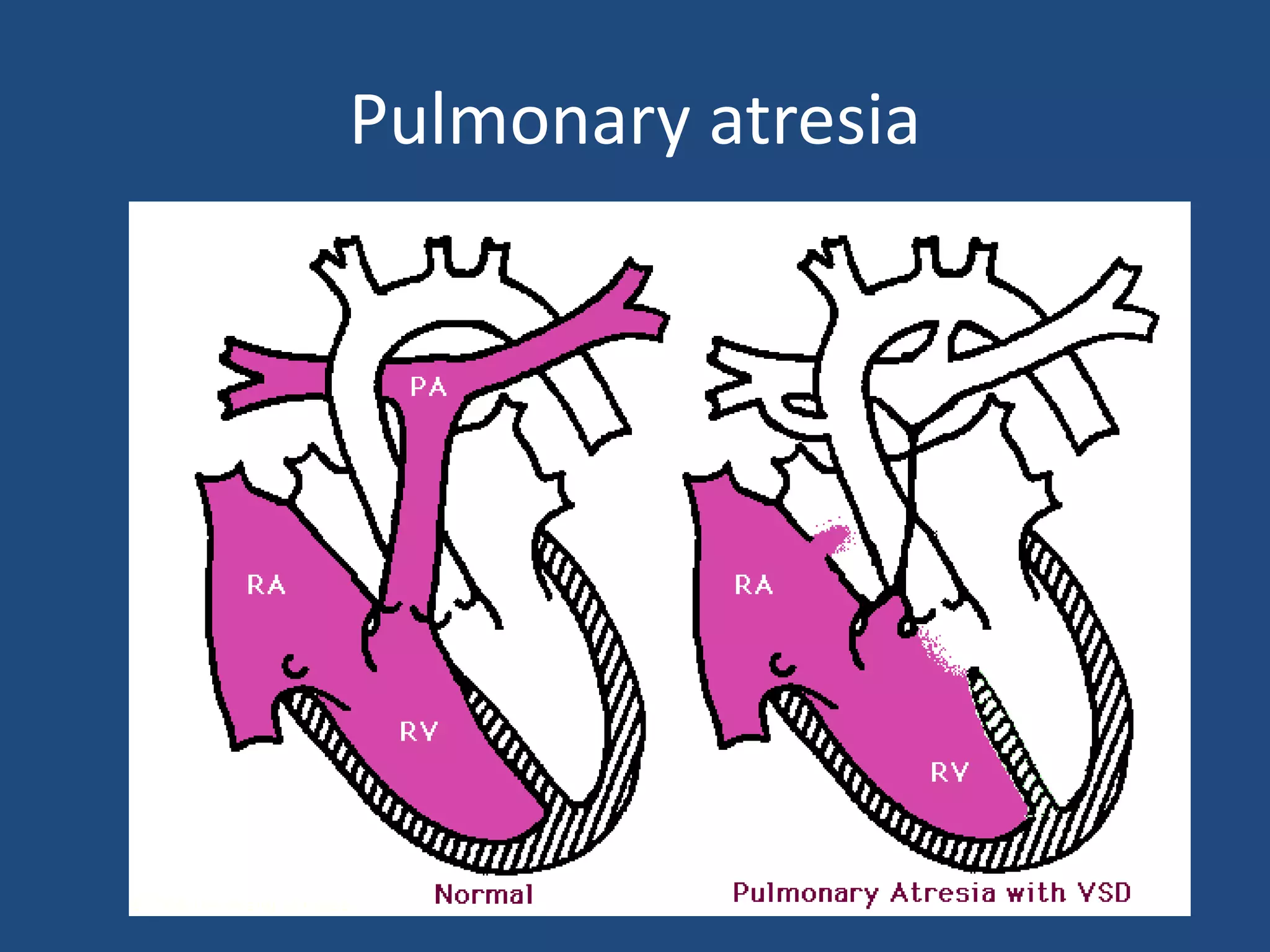
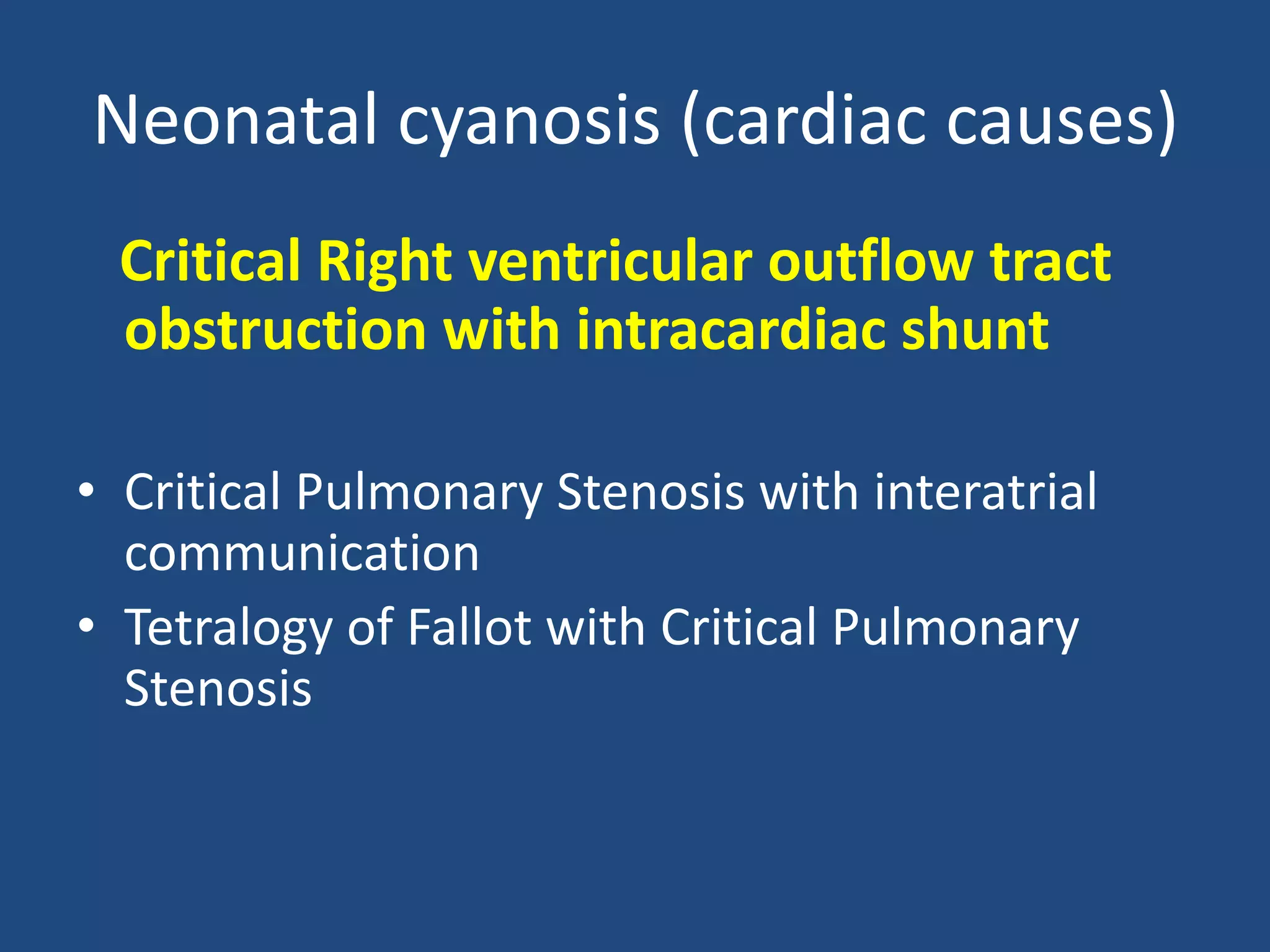
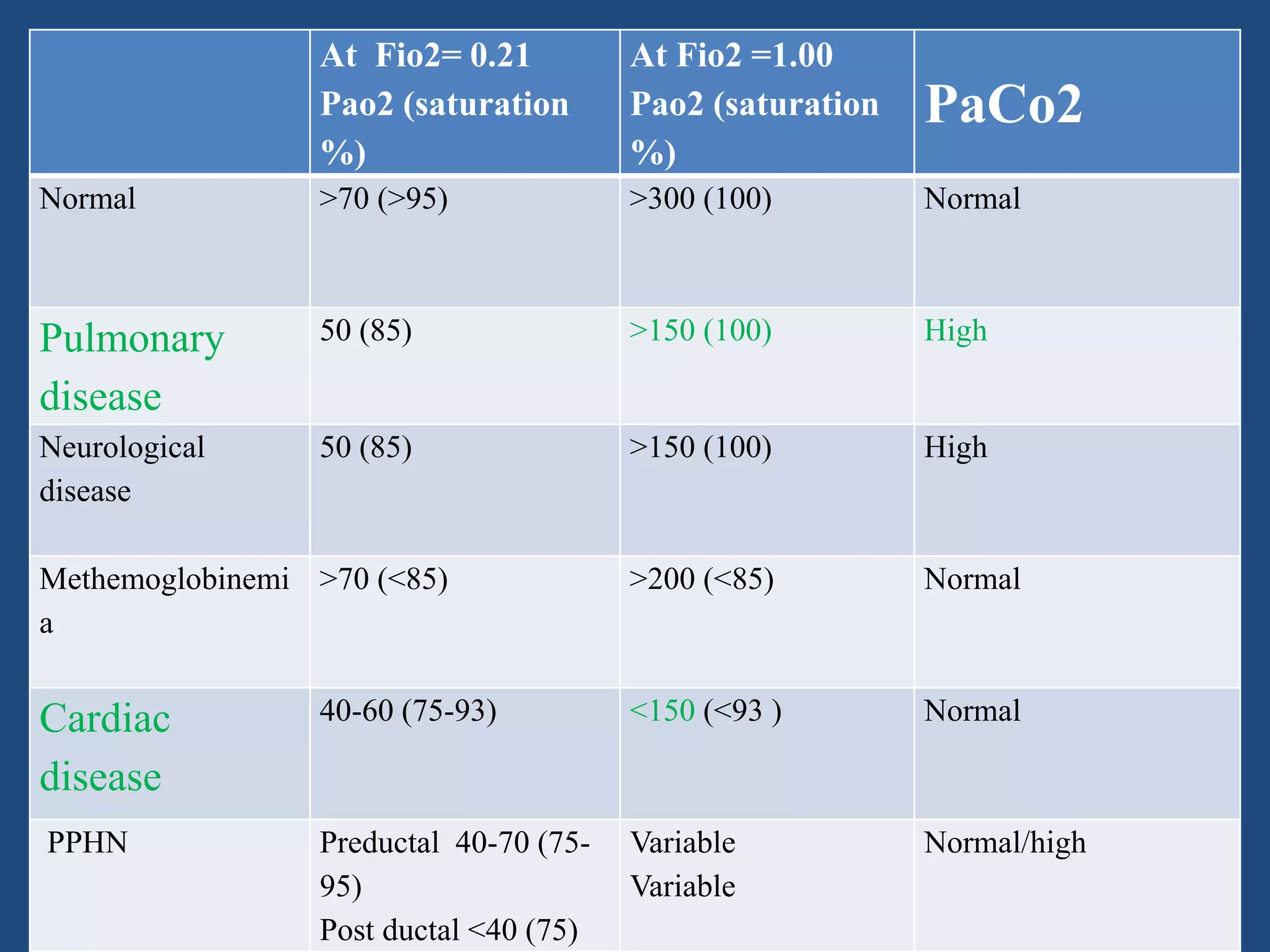
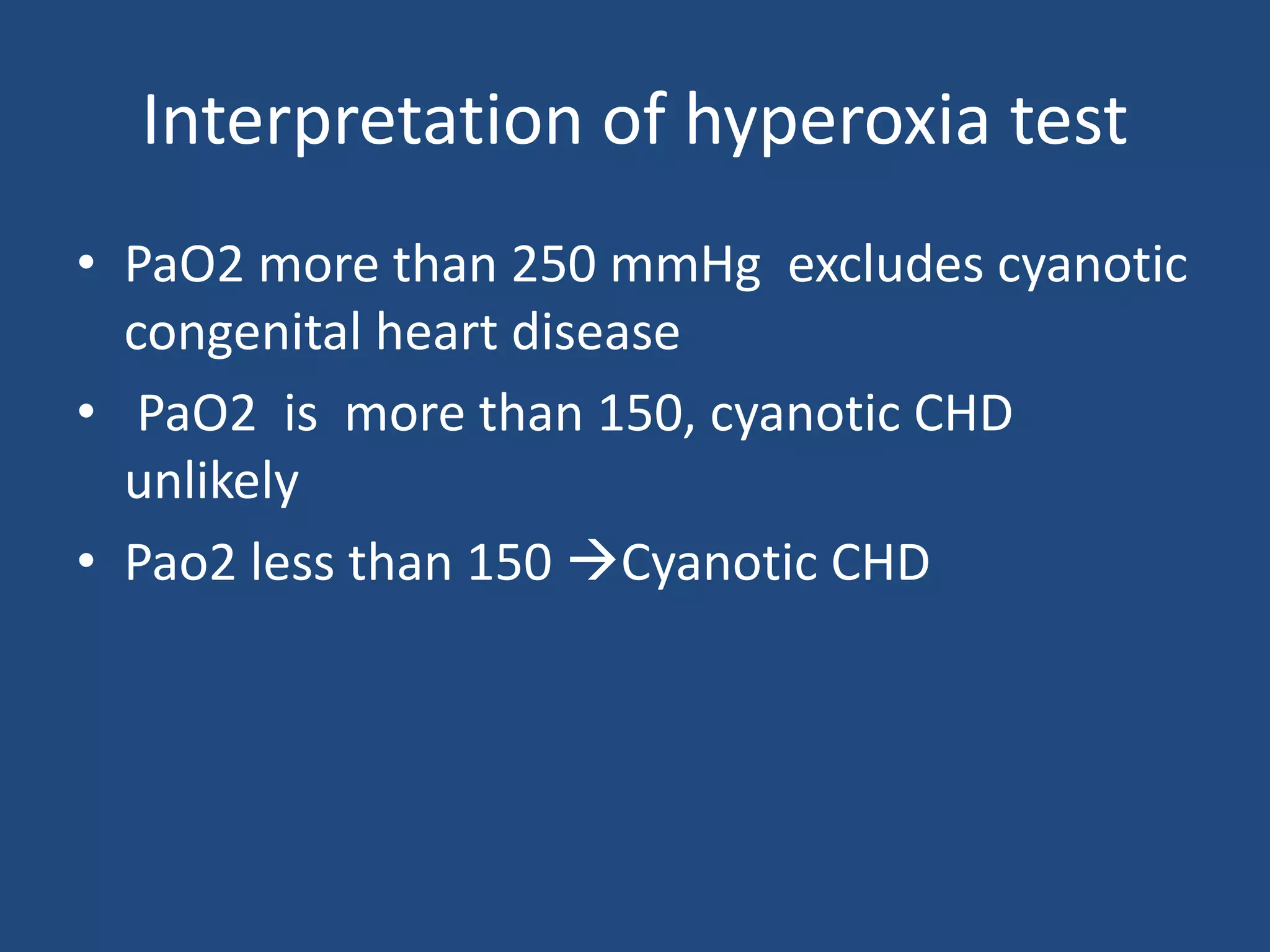
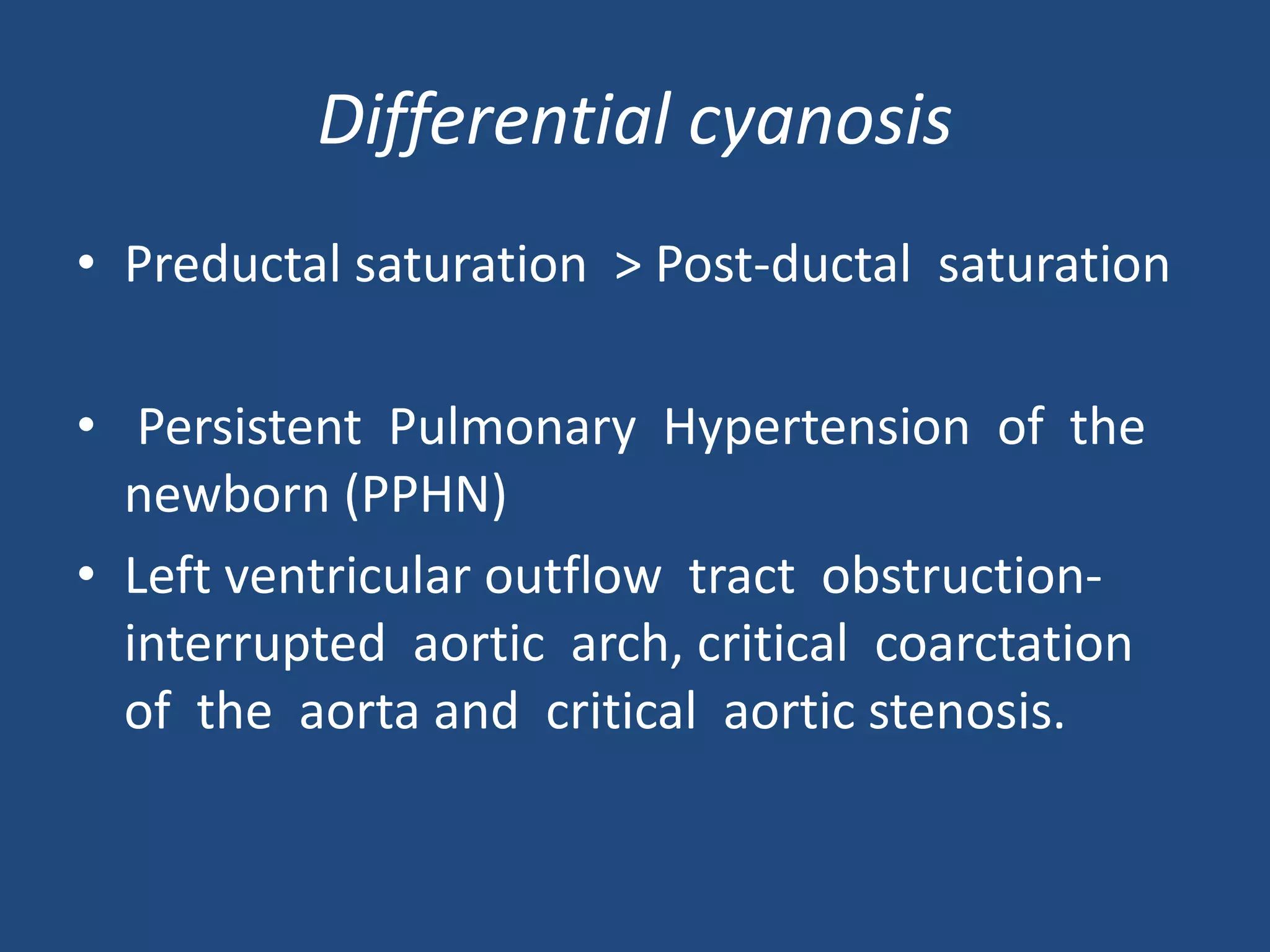
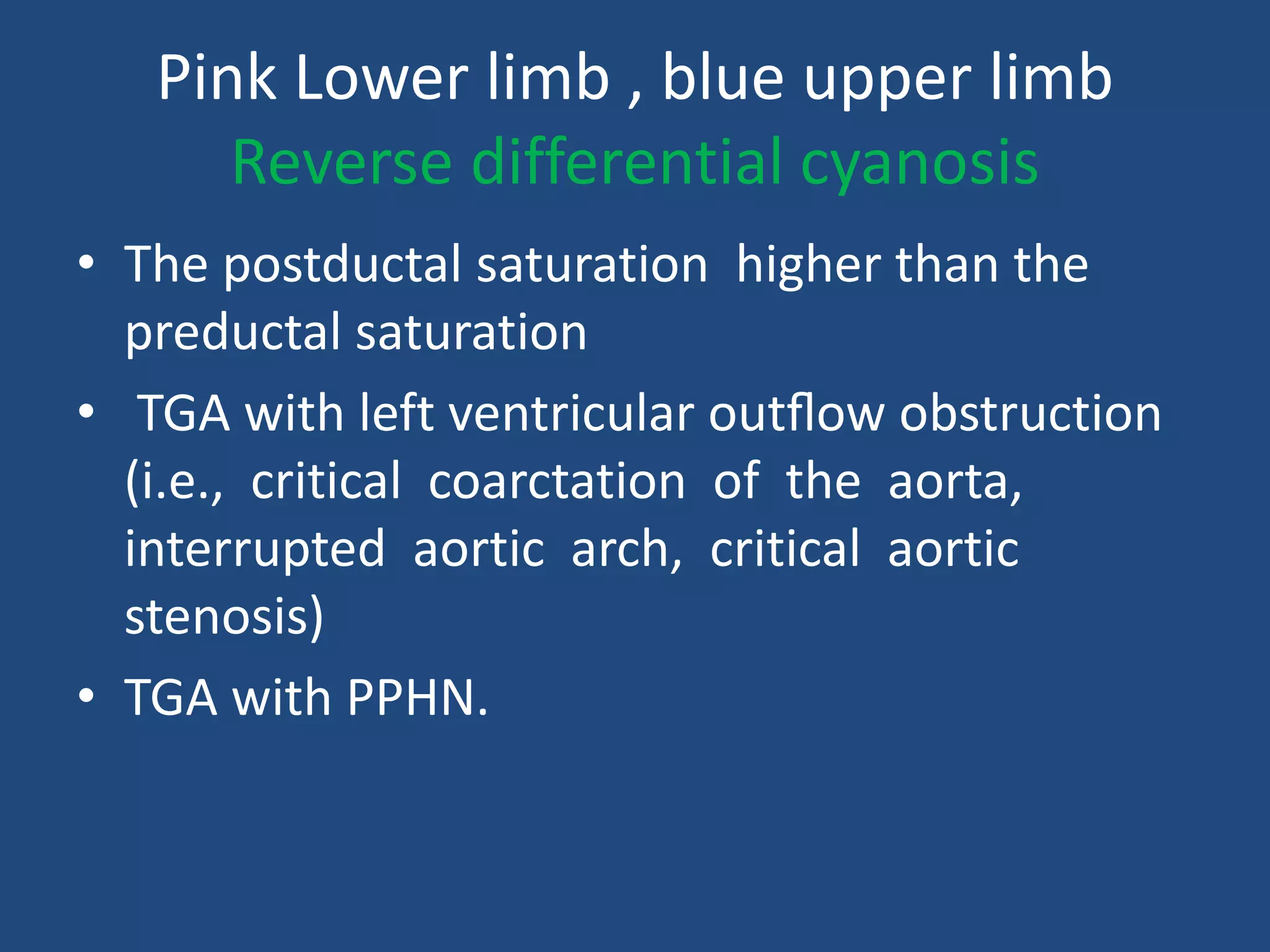
The document discusses neonatal cardiac emergencies, focusing on conditions like cyanosis, shock, and acute heart failure in newborns. It outlines various case studies and diagnostic techniques, emphasizing the importance of tools like the hyperoxia test and echocardiography for accurate diagnosis. The document also details management strategies including the use of prostaglandin E1 and various interventions for treating congenital heart defects.