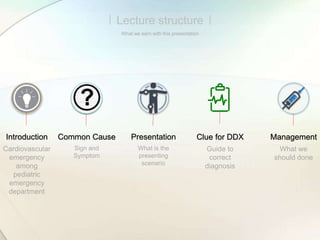
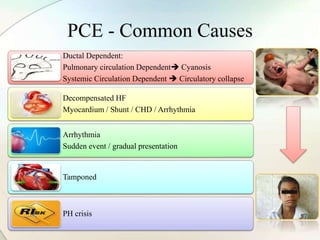
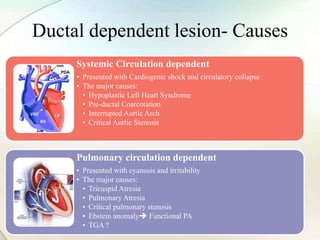
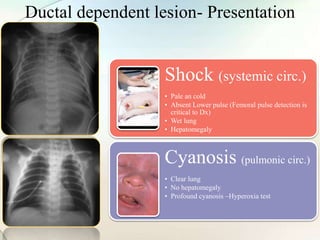
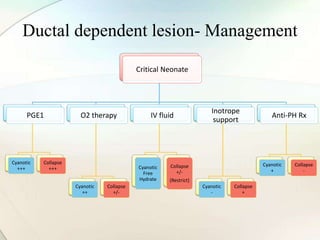
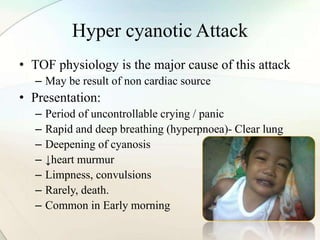
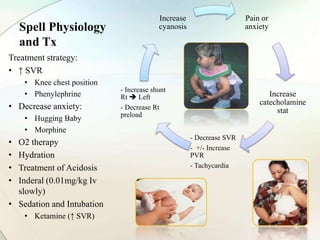
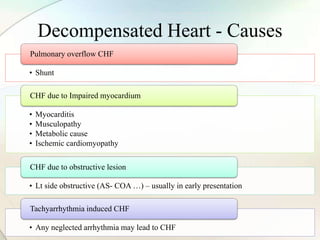
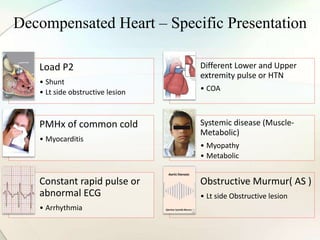
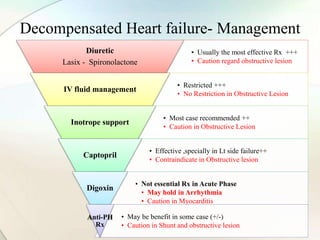
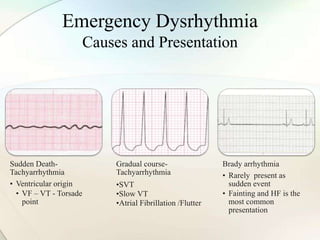
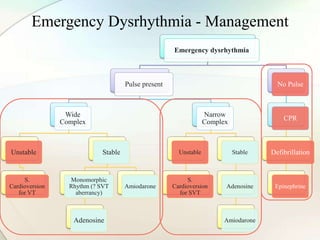
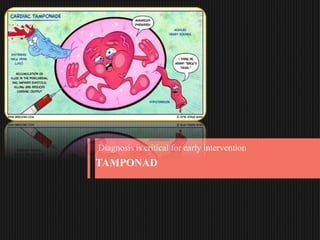
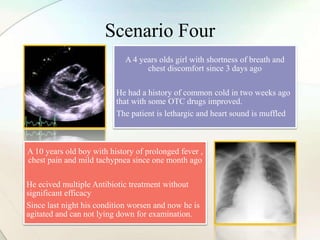
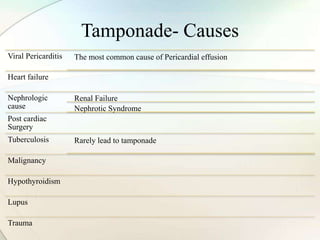
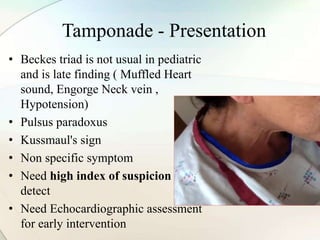
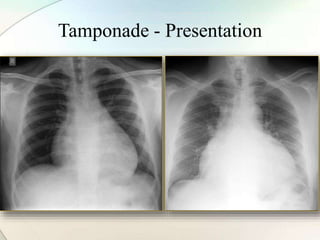
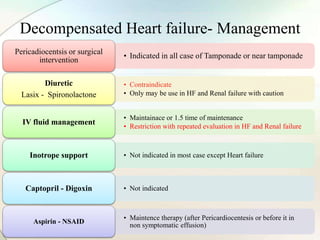
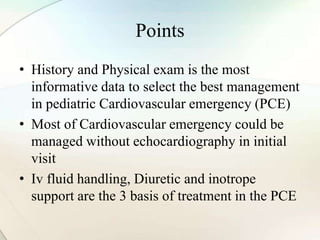
The document outlines an approach to pediatric cardiovascular emergencies, emphasizing the complexities of cardiac issues in children, which can be congenital or acquired. It provides detailed management strategies for various conditions such as ductal-dependent lesions, decompensated heart failure, emergency dysrhythmias, and cardiac tamponade. The document highlights the importance of history, physical examination, and initial management without relying solely on echocardiography.