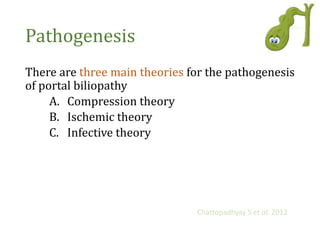
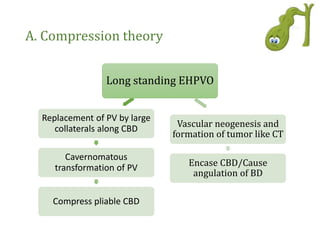
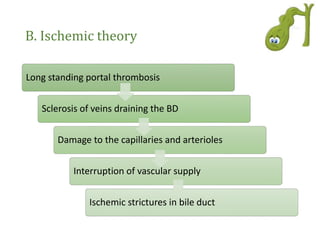
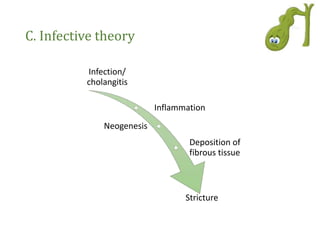
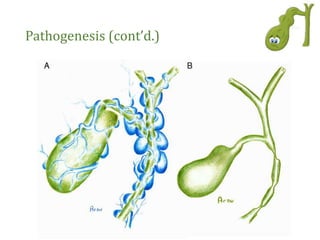
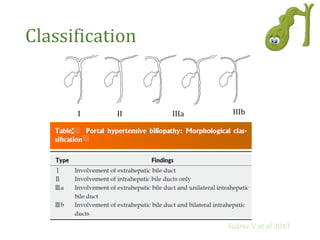
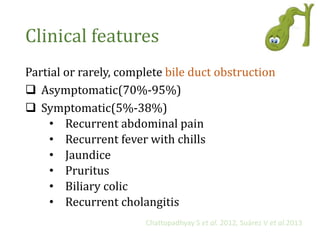
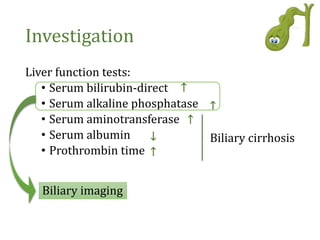
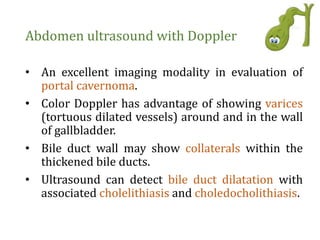
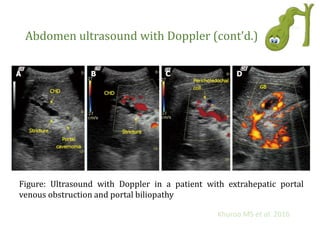
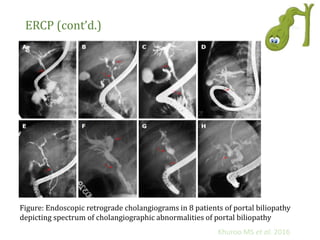
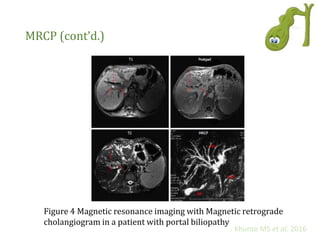
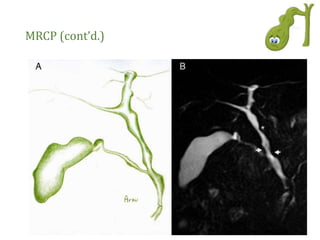
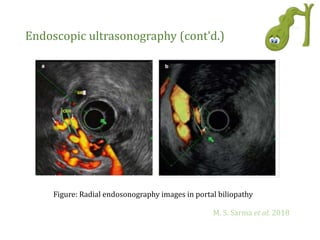
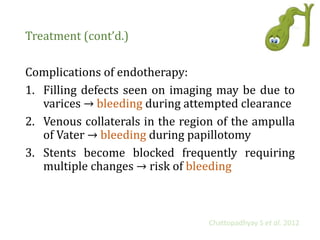
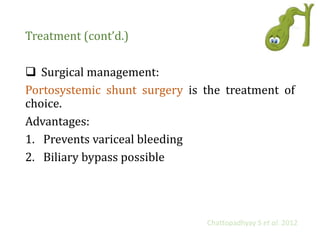
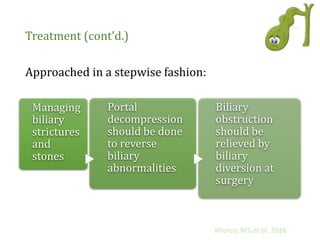
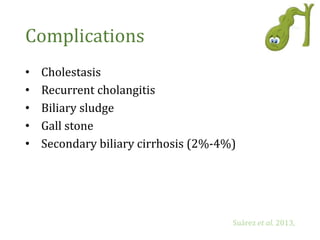
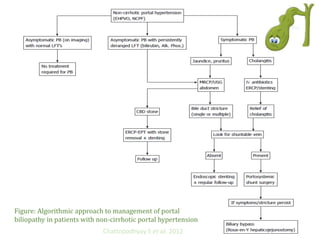
Portal biliopathy is a condition characterized by abnormalities in the biliary tract due to portal hypertension, particularly affecting patients with extrahepatic portal vein obstruction. Symptoms can include abdominal pain, jaundice, and cholangitis, with diagnosis primarily via imaging techniques such as ERCP and MRCP. Treatment varies based on symptoms, ranging from medical management for asymptomatic cases to surgical interventions for symptomatic patients.