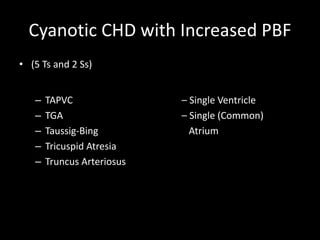
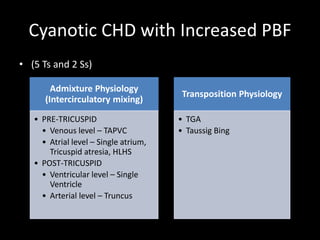
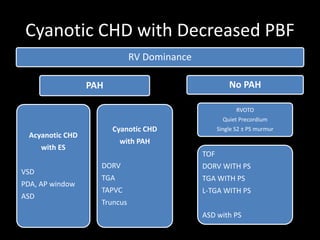
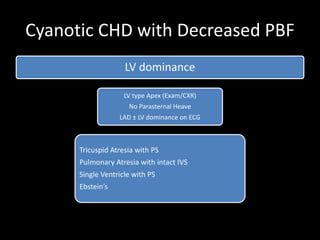
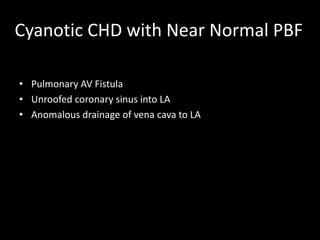
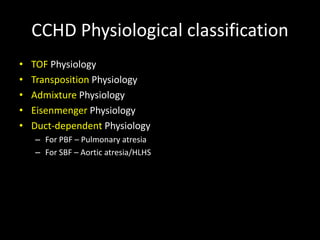
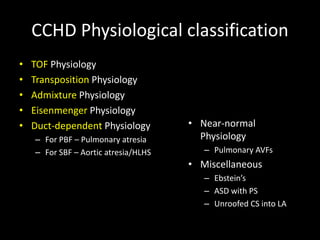
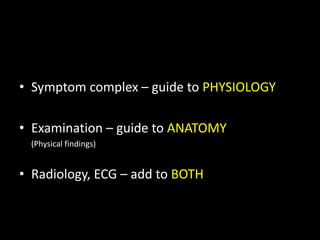
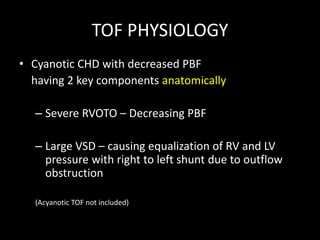
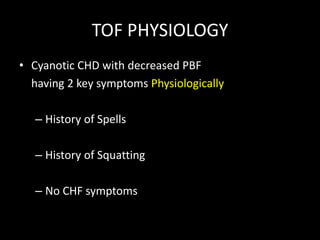
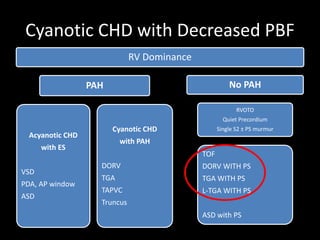
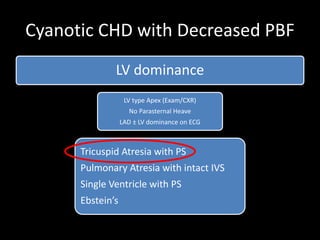
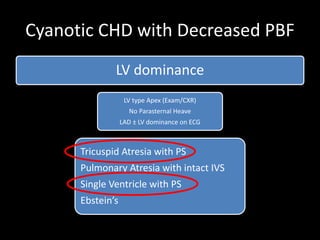
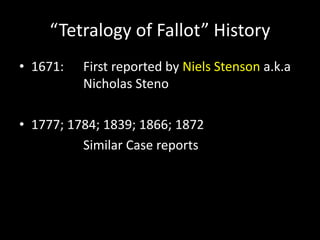
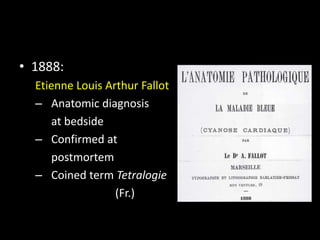
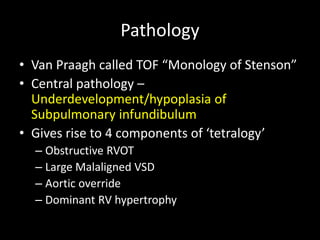
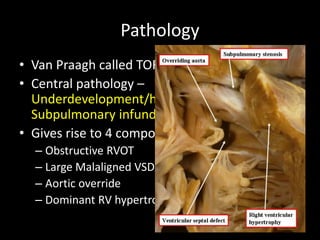
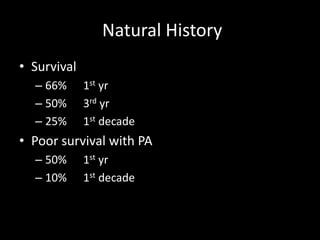
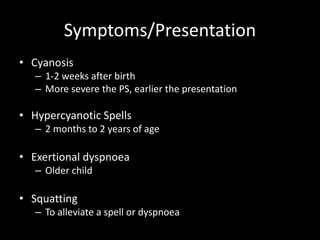
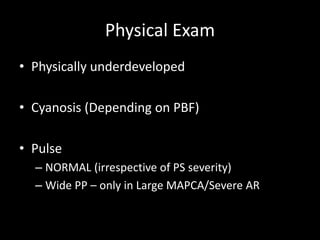
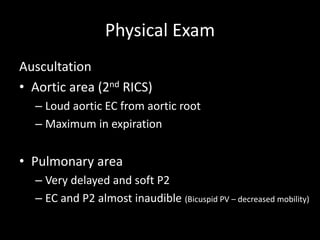
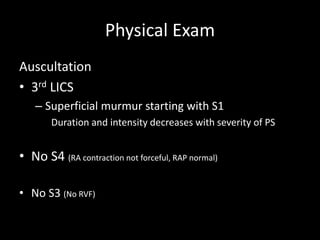
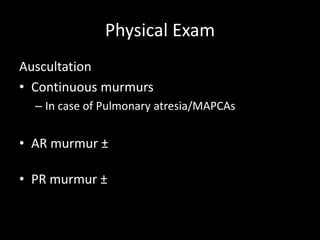
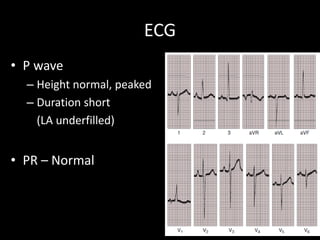
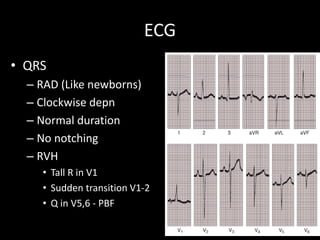
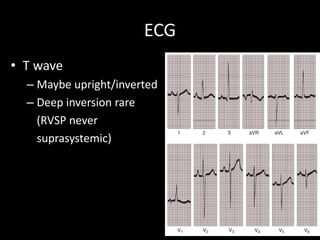
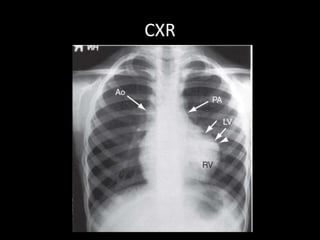
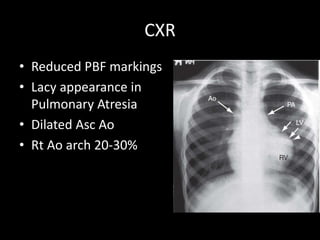
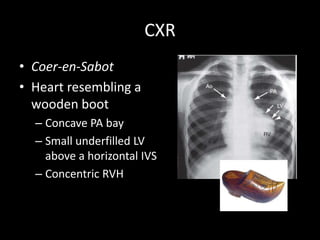
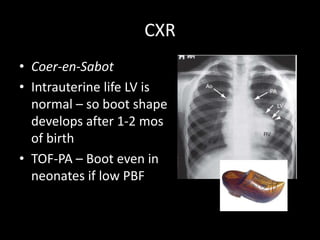
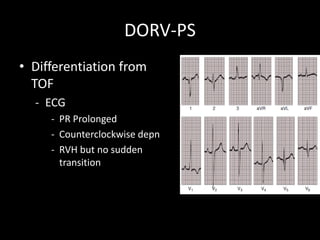
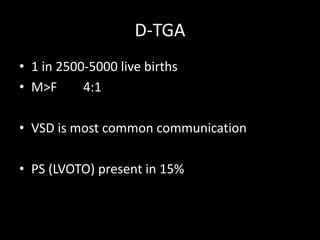
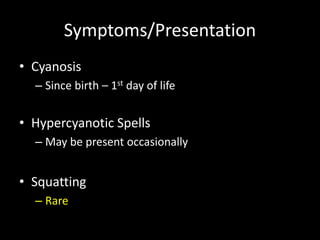
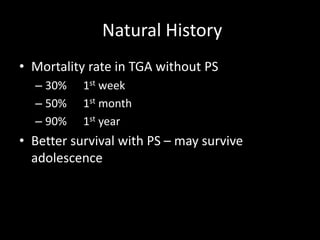
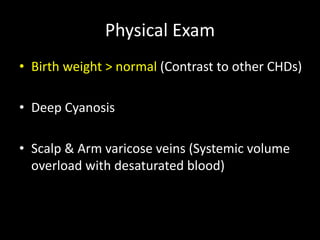
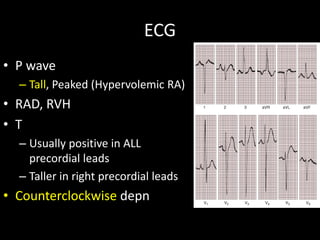
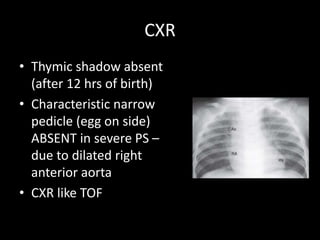
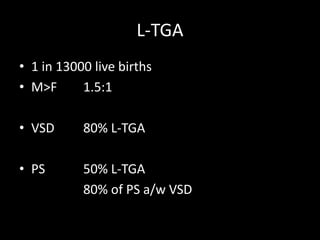
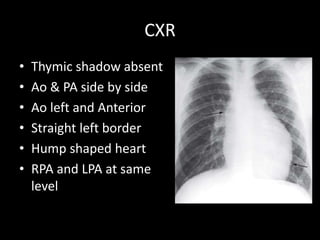
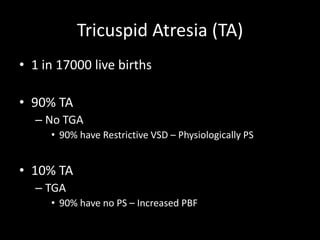
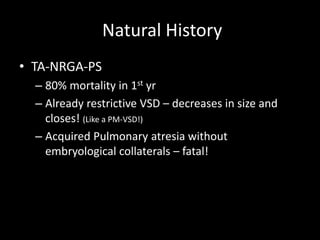
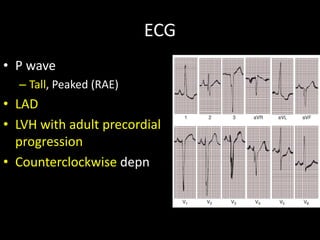
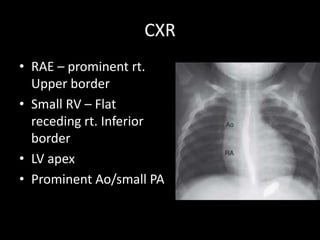
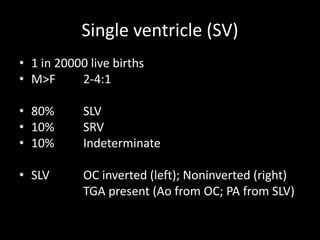
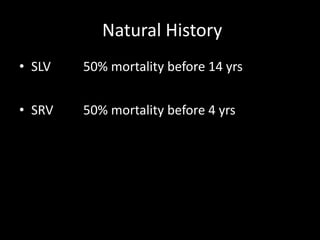
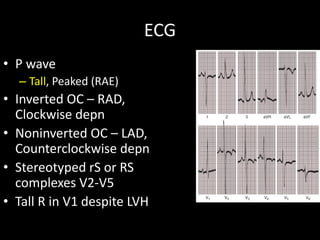
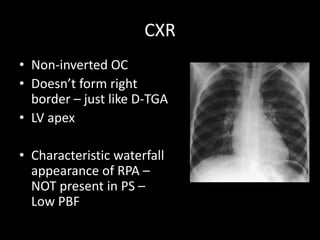
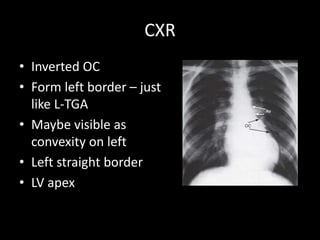
The document provides a detailed overview of the differential diagnosis and physiological classifications of cyanotic congenital heart disease (CHD), including several specific conditions like tetralogy of Fallot (ToF), transposition of great arteries (TGA), and tricuspid atresia. It discusses the symptoms, presentations, natural history, and physical exam findings associated with each condition, along with their respective diagnostic implications. Emphasis is placed on the anatomical and physiological characteristics, along with the historical context of these congenital defects.