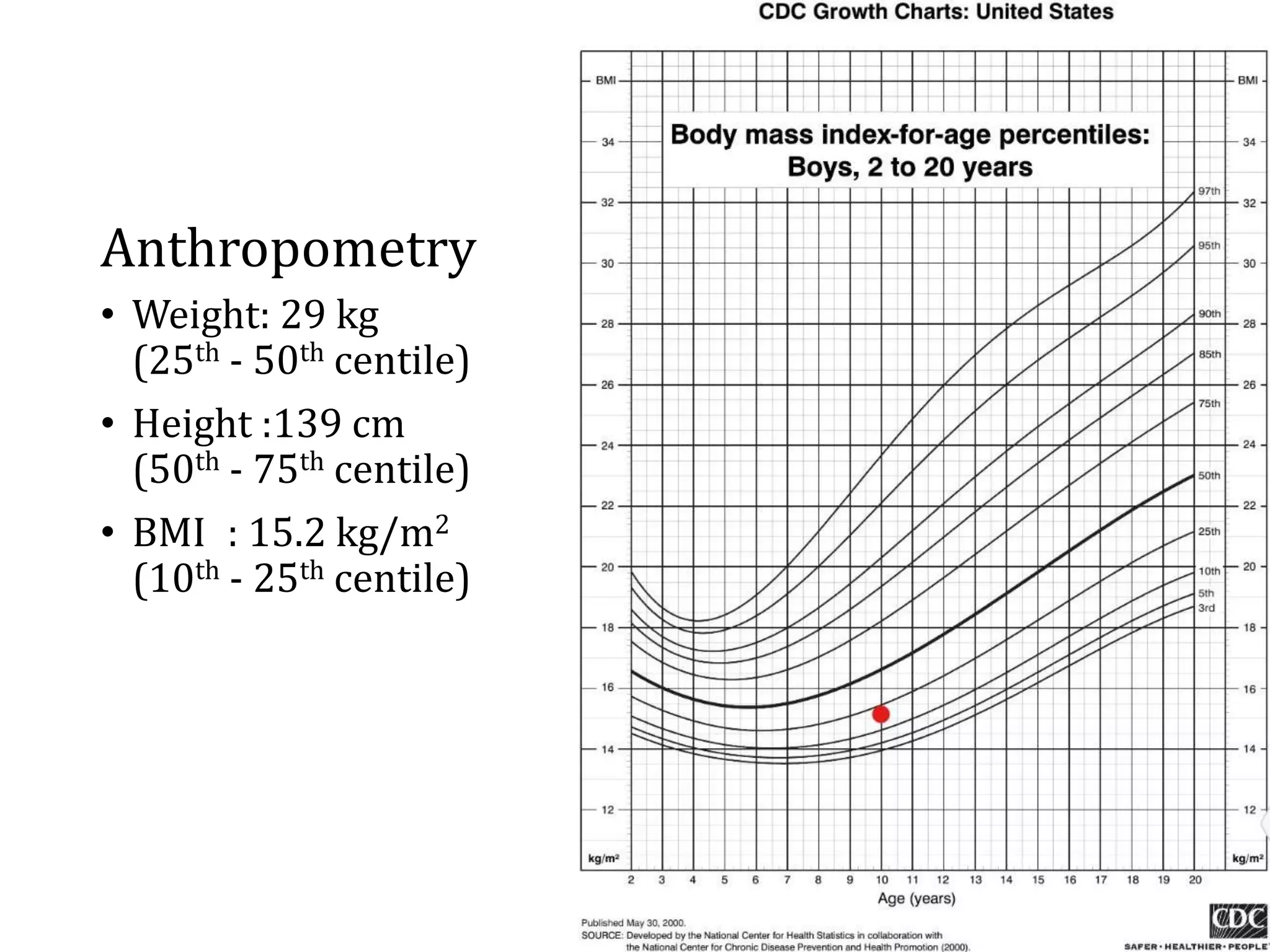
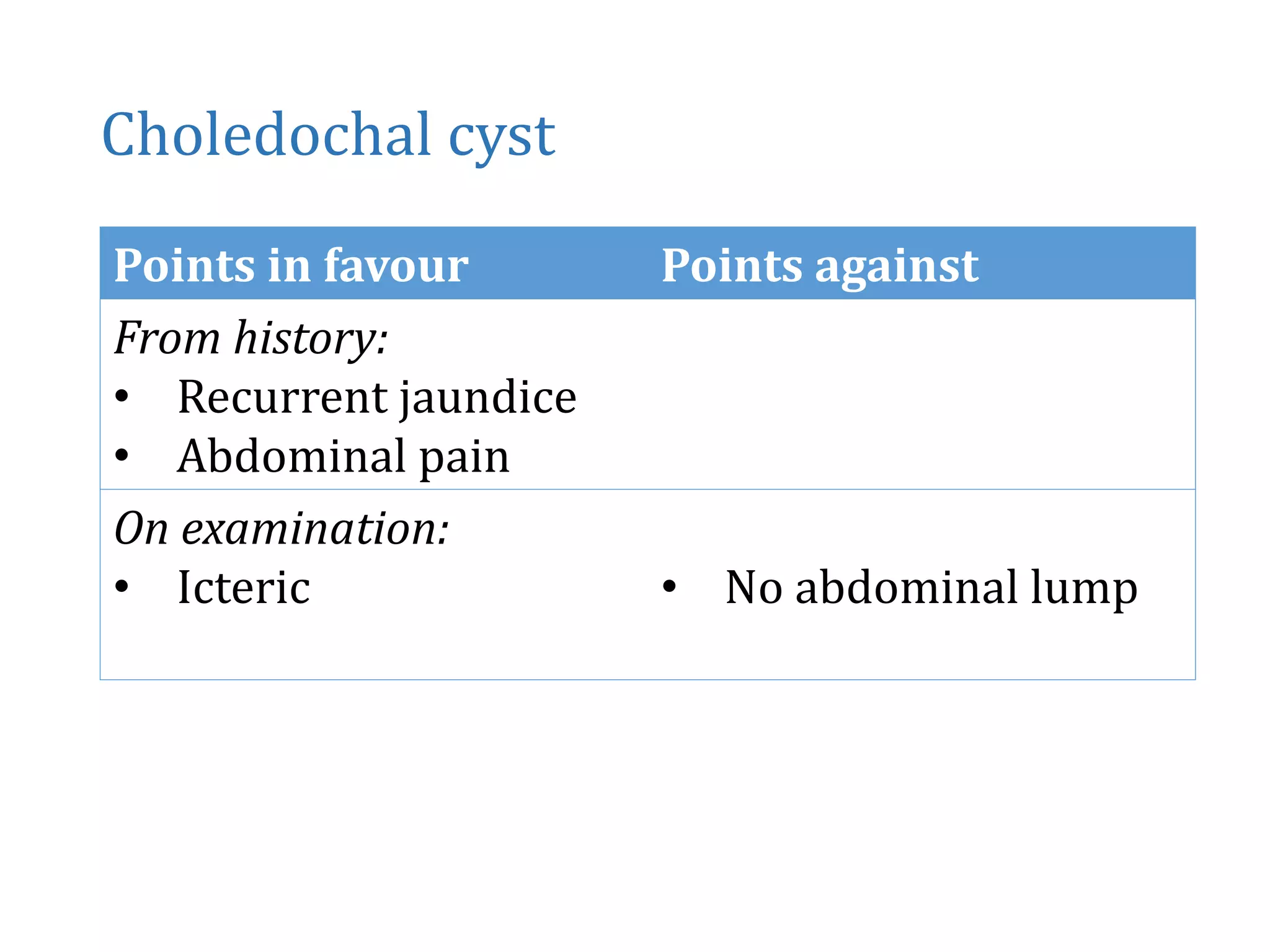
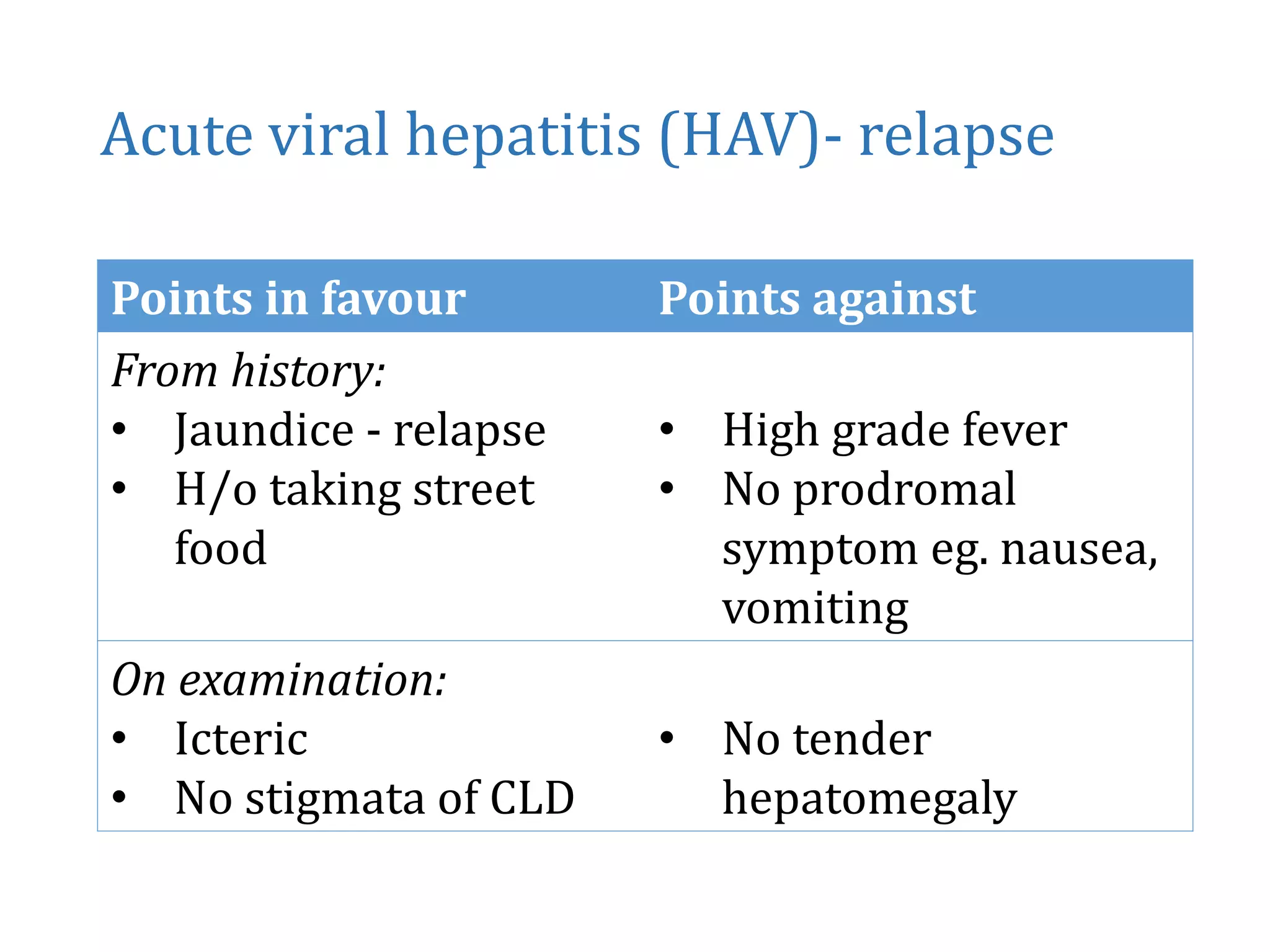
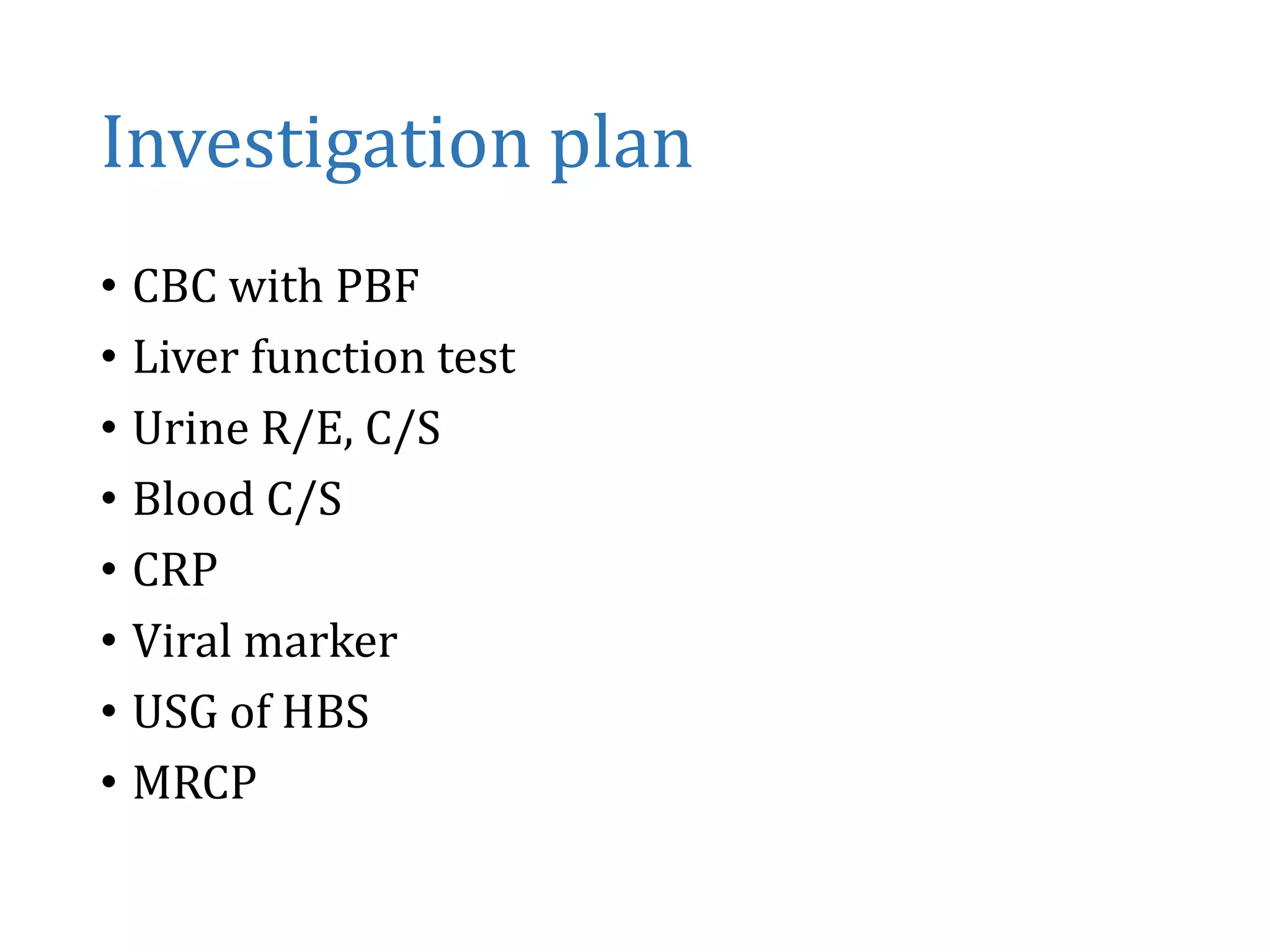
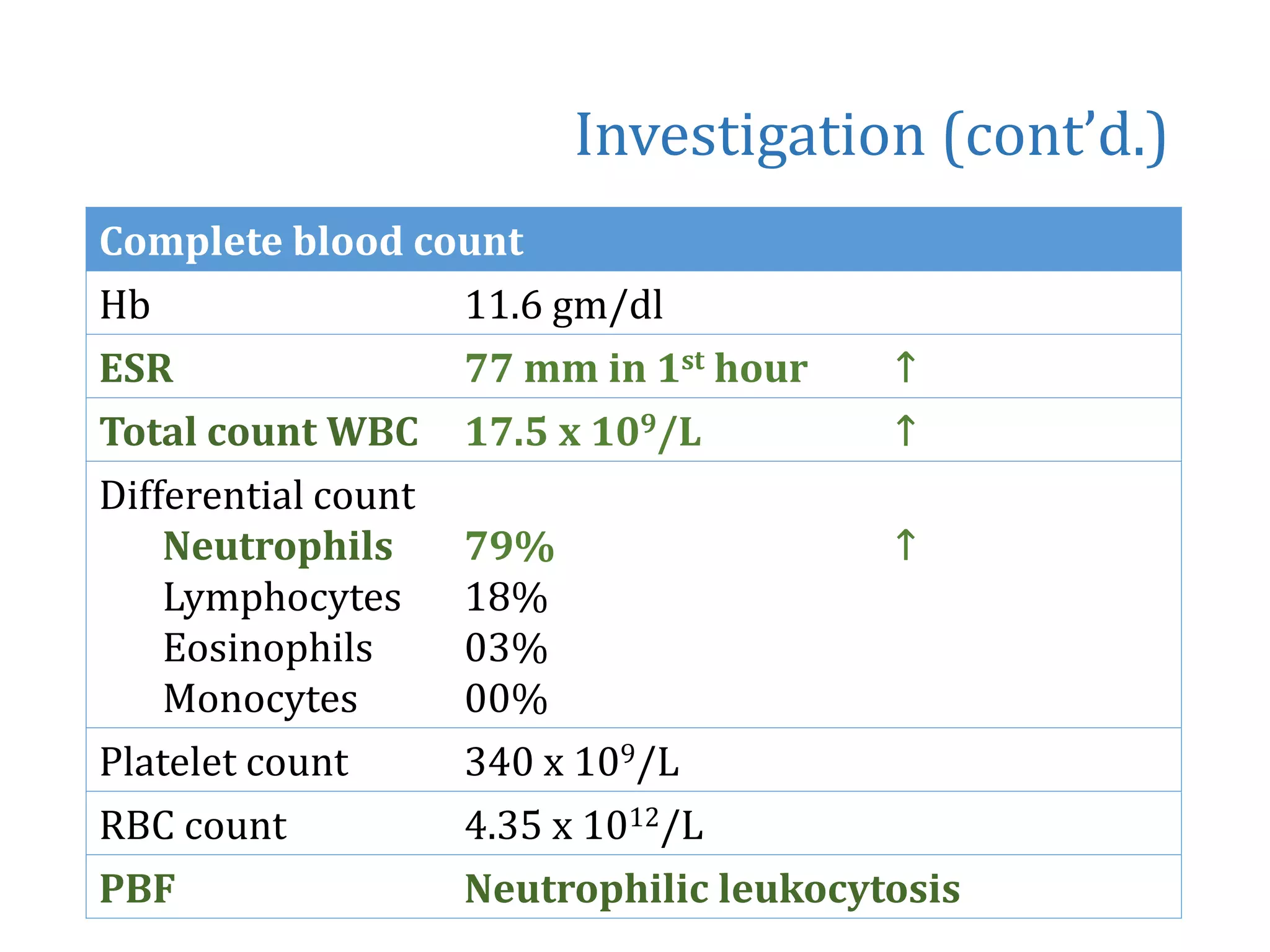
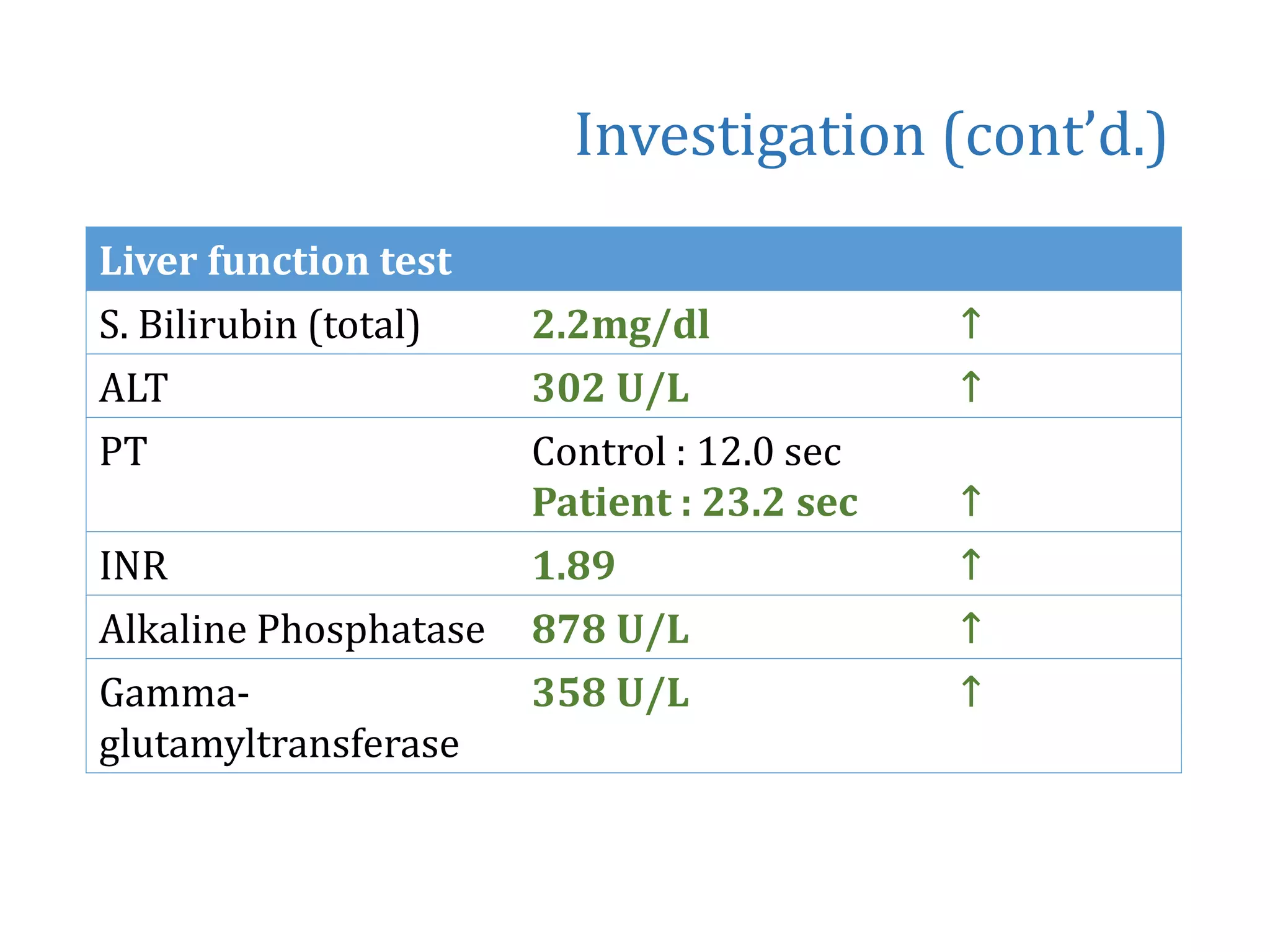
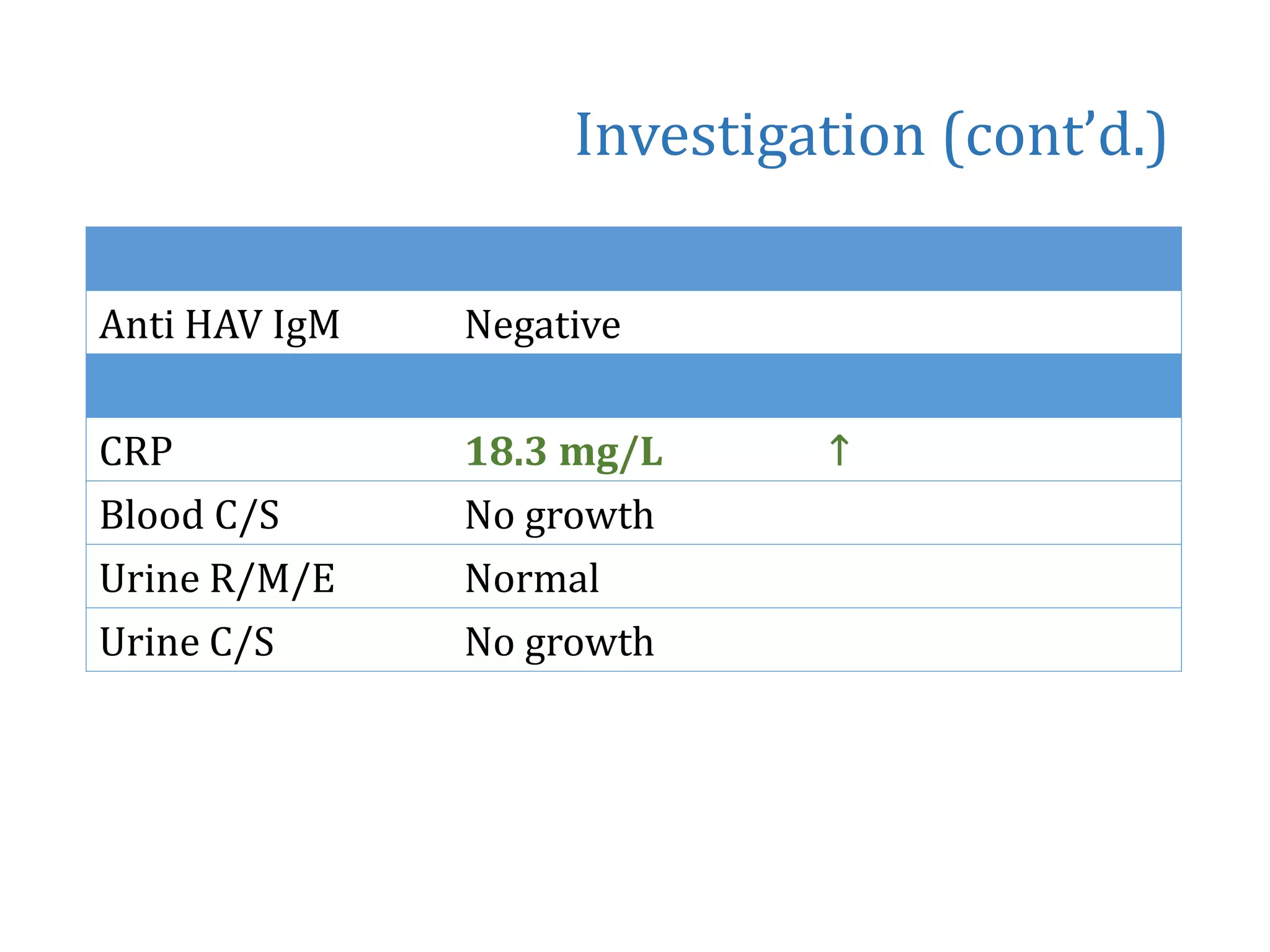
The document summarizes the case of a 10-year-old boy admitted with fever, jaundice, and abdominal pain. Key findings include intermittent high fever for 4 days, jaundice for 4 days, and occasional right upper abdominal pain. He had a similar prior episode 2 months ago. Examination found him febrile but otherwise stable. Tests showed elevated liver enzymes and bilirubin. Ultrasound and MRCP found a fusiform dilated common bile duct suggestive of a choledochal cyst. He was started on antibiotics and vitamin K. His fever subsided after a few days but jaundice remained. A pediatric surgery consultation was requested.