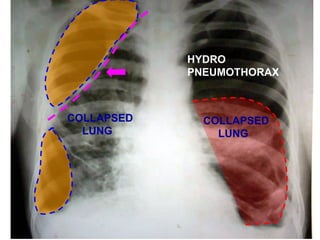
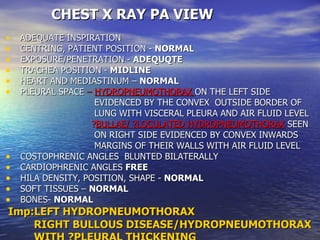
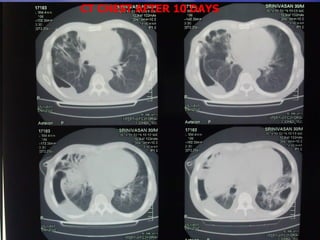
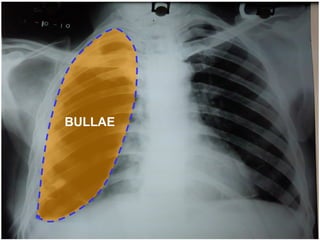
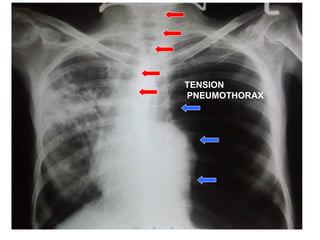
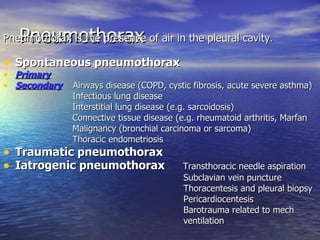
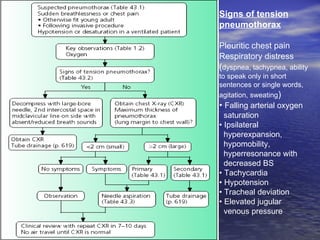
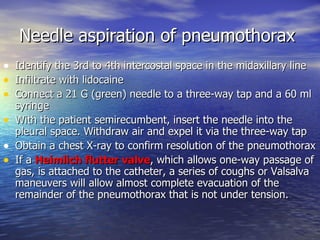
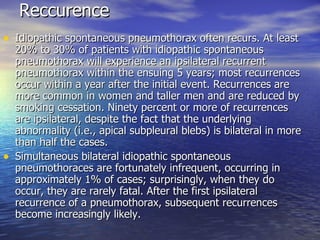
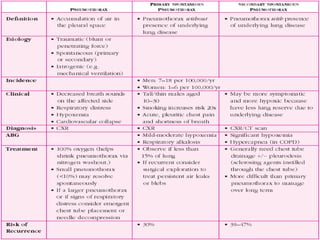
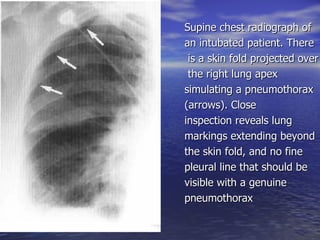
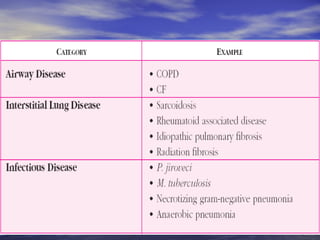
A 30-year-old male presented with complaints of breathlessness and cough with expectoration for one month. Chest X-ray and CT scan revealed left hydropneumothorax, right bullous disease/hydropneumothorax, and bilateral lower lobe bronchiectasis. Needle aspiration was performed to relieve the pneumothorax. Idiopathic spontaneous pneumothorax often recurs, with at least 20-30% experiencing recurrence within 5 years, usually within the first year. Distinguishing features between a skin fold and genuine pneumothorax on chest X-ray include lung markings extending beyond the fold and absence of a fine pleural line.