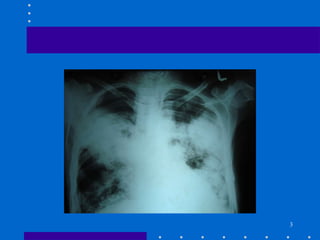
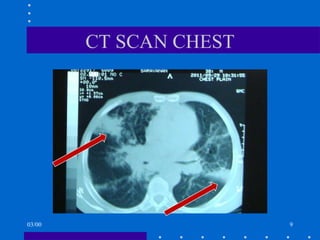
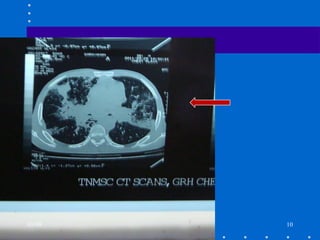
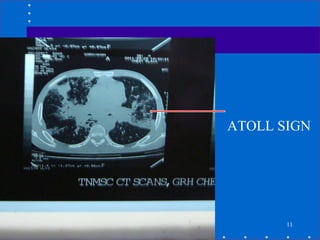
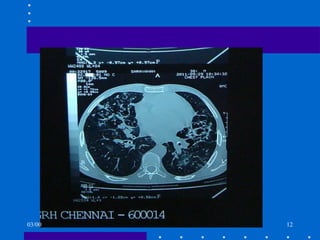
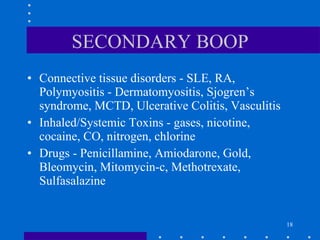
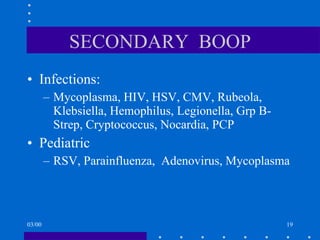
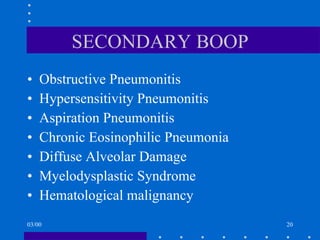
A 28-year-old male presented with cough, dyspnea, fever, malaise, and weight loss. Chest X-ray and CT scan showed bilateral heterogeneous airspace opacities. He did not improve with antibiotics but responded well to steroids, suggestive of idiopathic bronchiolitis obliterans organizing pneumonia (BOOP). BOOP is a non-specific inflammatory reaction of small airways that can be idiopathic or secondary to various causes. It is treated with steroids and immunosuppressants if unresponsive to steroids.