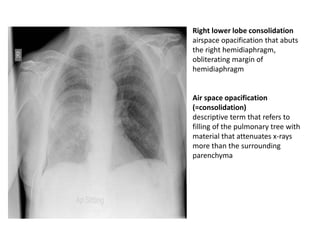
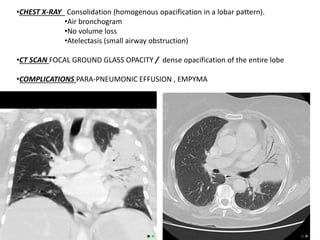
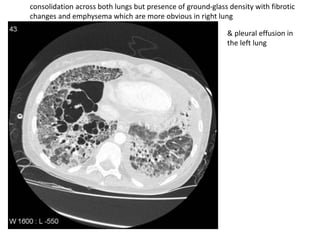
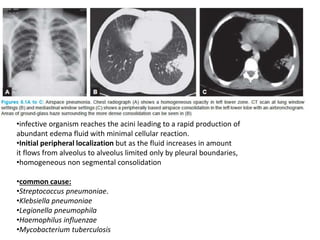
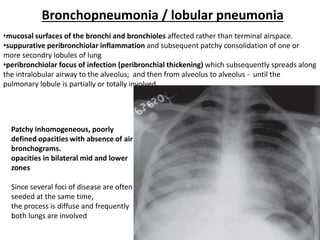
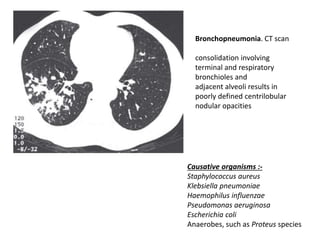
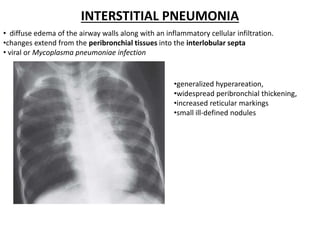
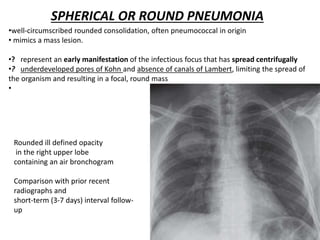
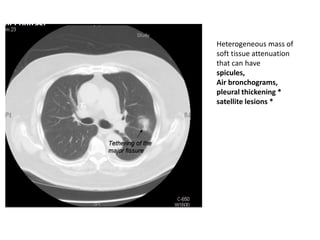
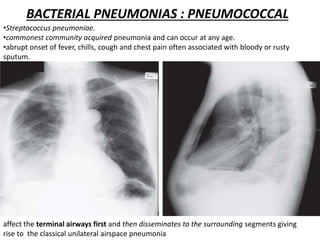
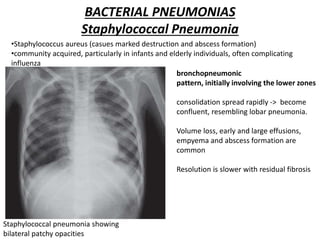
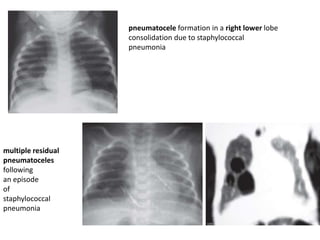
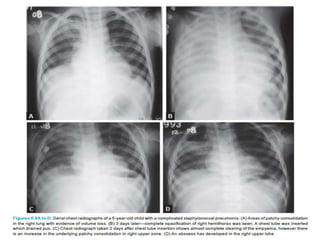
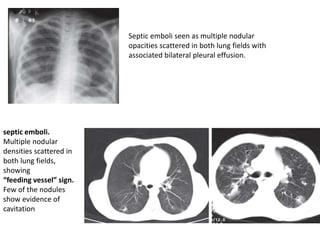
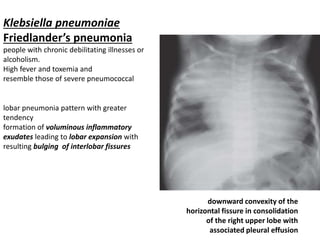
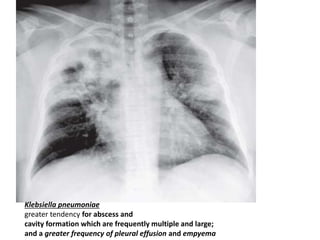
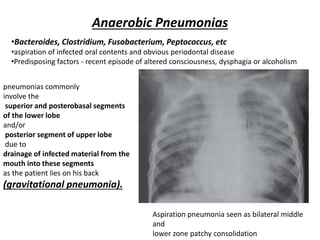
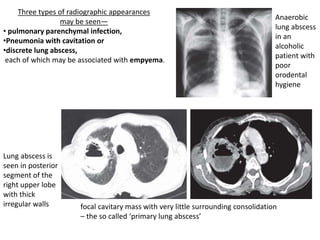
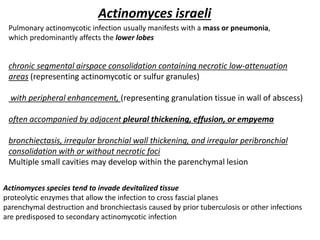
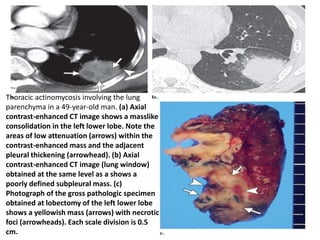
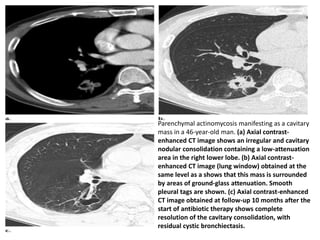
This document summarizes various types of non-tubercular pulmonary infections seen on imaging. It describes the common radiographic appearances of different bacterial, fungal and parasitic pneumonias on chest x-rays and CT scans. Key findings include lobar/lobular consolidations, air bronchograms, cavitations, nodules, ground glass opacities and pleural effusions seen with specific pathogens like Streptococcus pneumoniae, Staphylococcus aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa, anaerobes and Actinomyces israeli. Imaging helps establish the diagnosis, locate the infection and assess treatment response or complications.