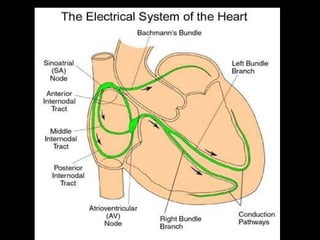
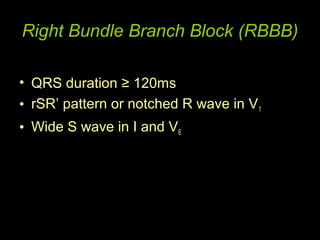
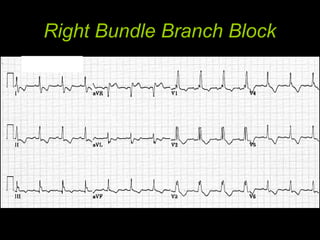
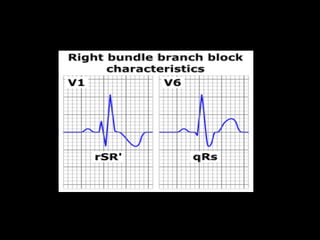
1) Right bundle branch block (RBBB) is characterized by a QRS duration ≥ 120ms and signs of delayed right ventricular activation. It is commonly benign but worsens prognosis when seen in acute myocardial infarction, especially of the proximal left anterior descending artery.
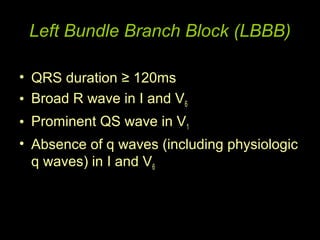
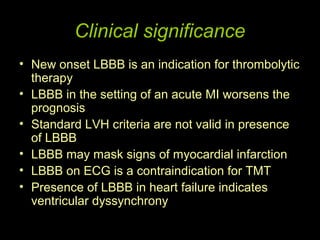
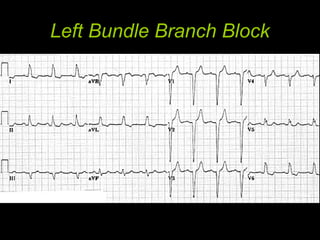
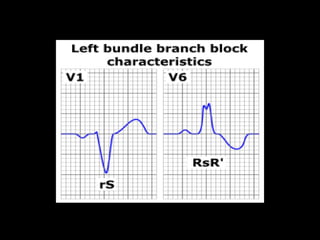
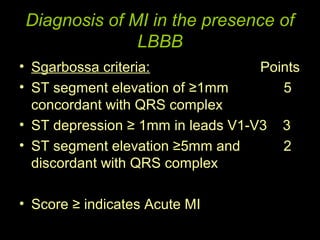
2) Left bundle branch block (LBBB) has a QRS duration ≥ 120ms and signs of delayed left ventricular activation. New onset LBBB indicates the need for thrombolysis in myocardial infarction and worsens prognosis when seen in acute myocardial infarction.
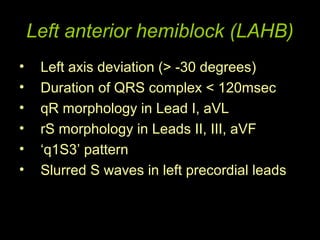
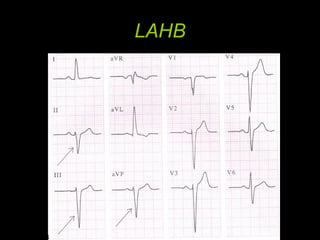
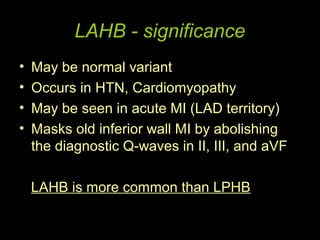
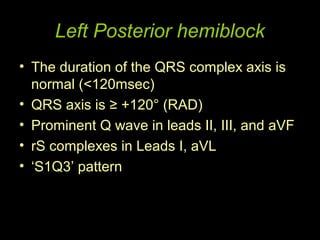
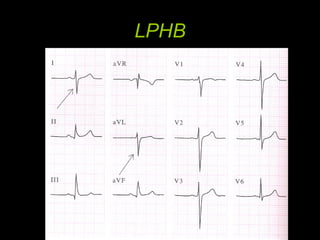
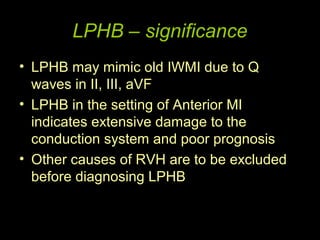
3) Hemiblocks involve delayed activation of only one side of the ventricles. Left anterior hemiblock may mask inferior wall myocardial infarction. Left posterior hemiblock in anterior myocardial infarction