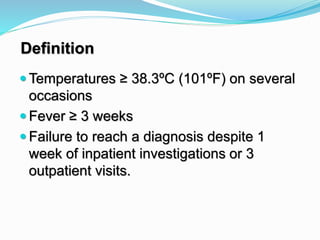
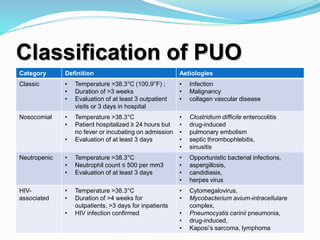
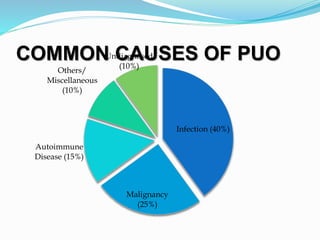
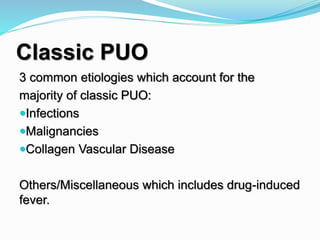
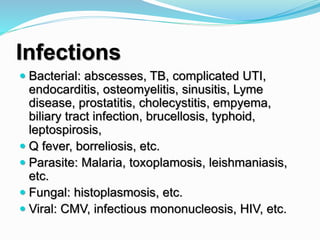
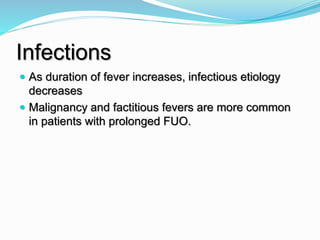
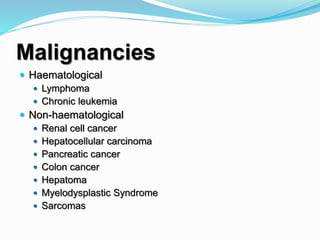
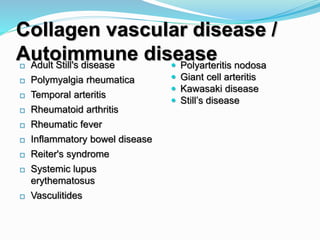
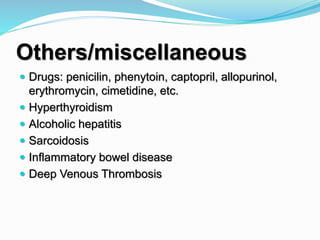
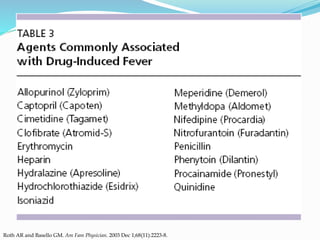
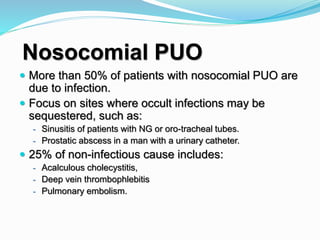
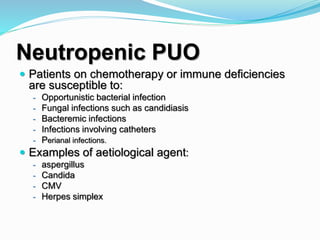
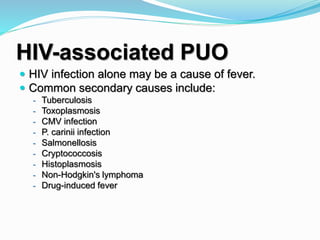
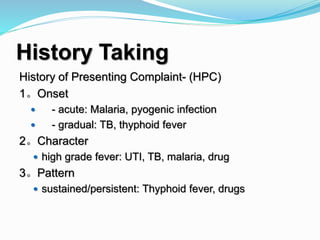
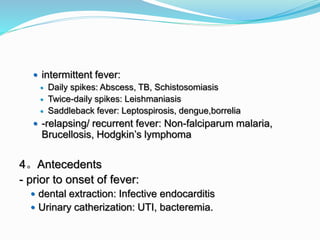
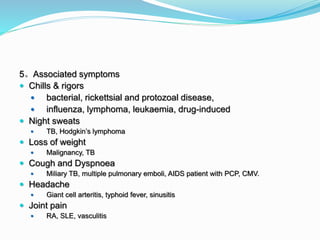
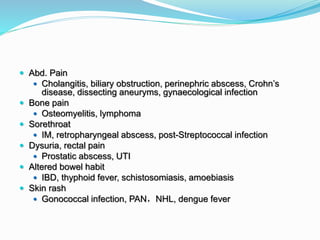
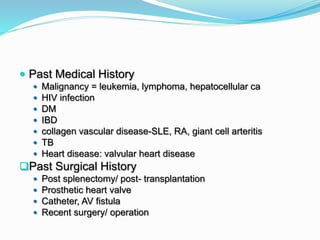
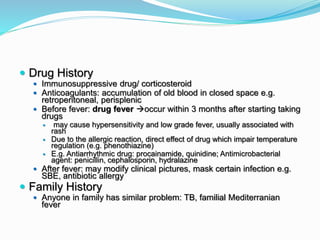
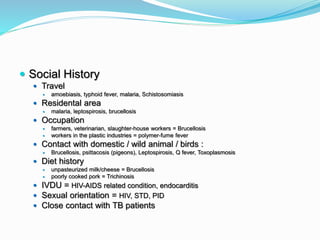
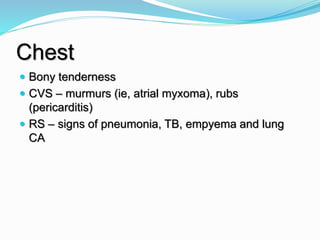
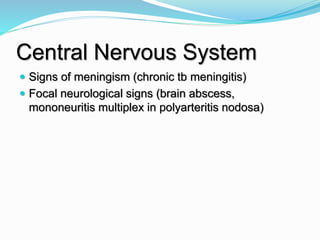
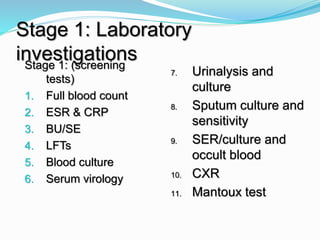
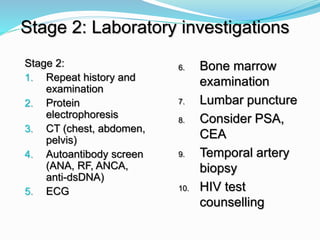
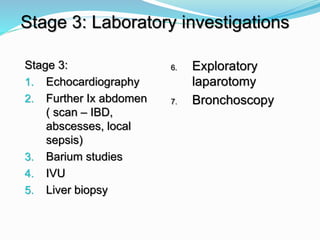
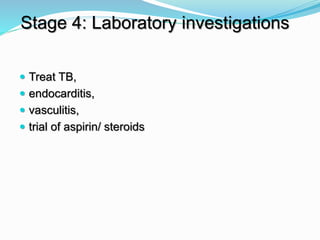
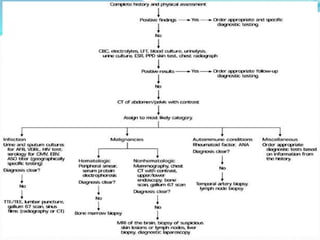
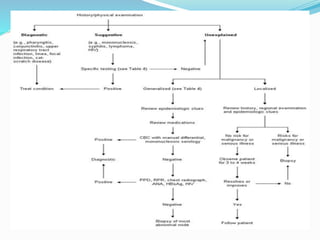
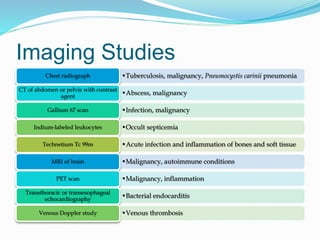
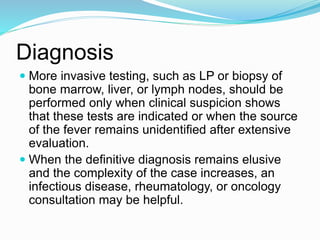
Dr. W.A.P.S.R.Weerarathna defines pyrexia of unknown origin (PUO) as a temperature of ≥ 38.3°C on multiple occasions for ≥ 3 weeks without reaching a diagnosis. Common causes of PUO include infections (40%), malignancies (25%), and autoimmune diseases (15%). For classic PUO, the three most common etiologies are infections, malignancies, and collagen vascular diseases. A thorough history, physical exam, and initial laboratory/imaging tests are recommended to guide further targeted investigations. More invasive testing should only be done if indicated or if initial evaluation does not identify the source of fever.