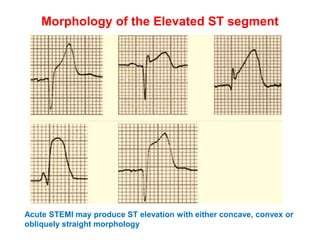
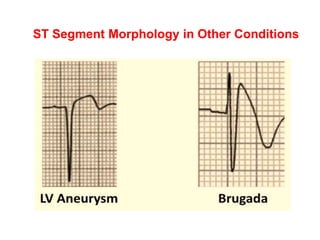
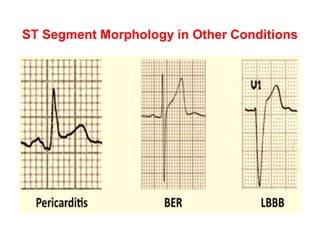
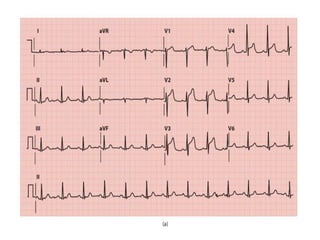
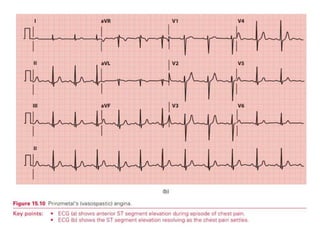
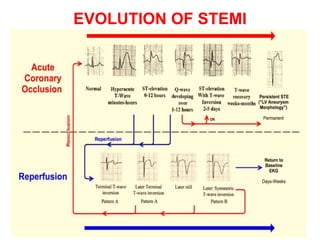
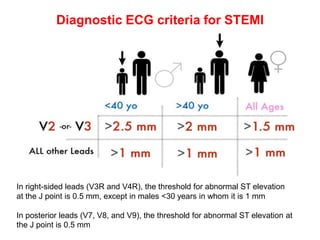
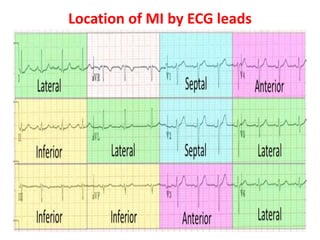
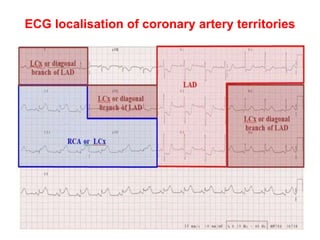
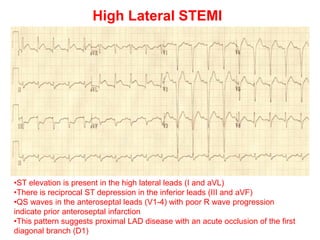
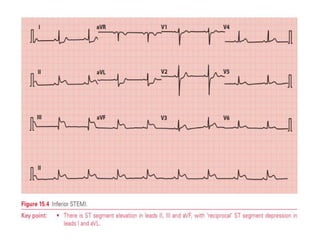
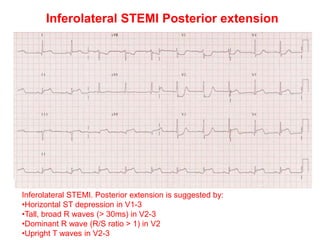
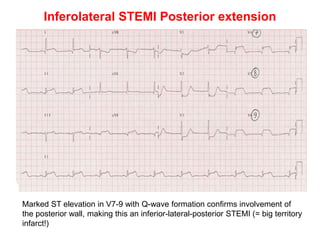
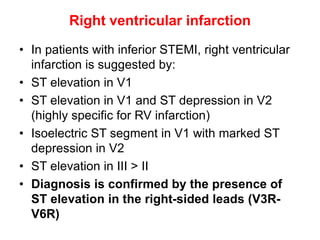
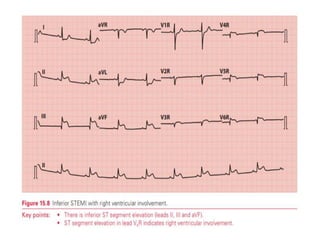
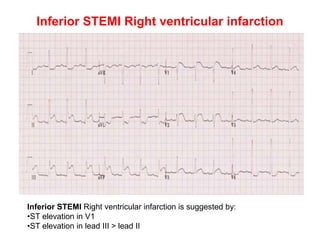
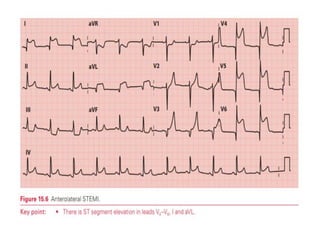
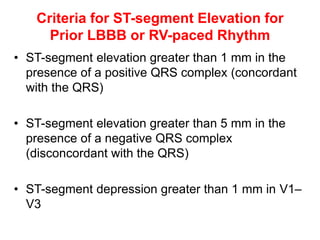
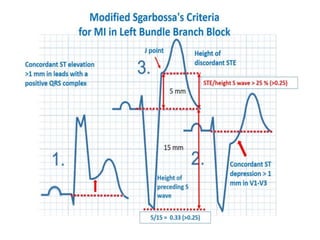
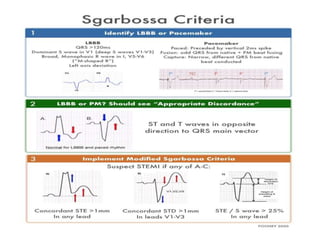
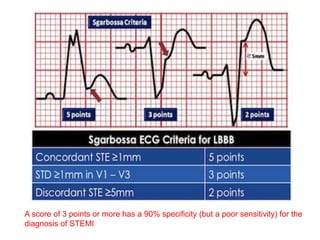
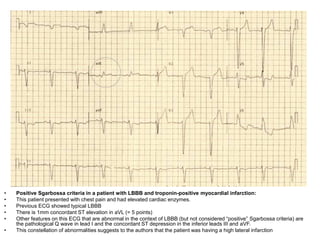
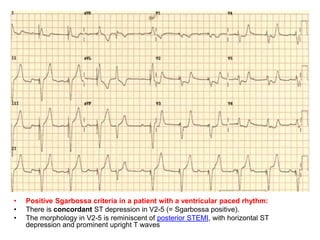
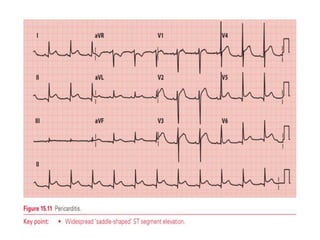
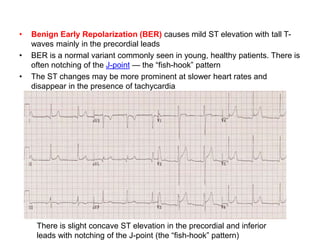
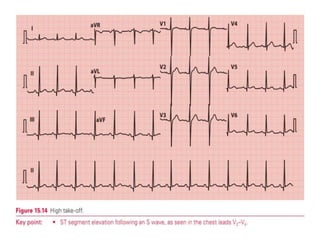
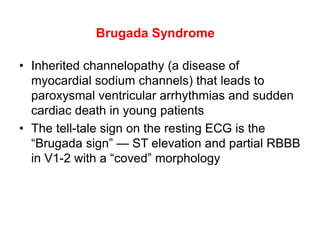
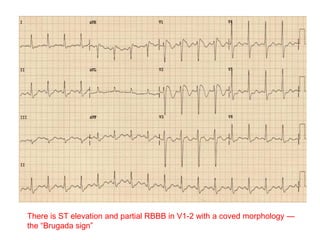
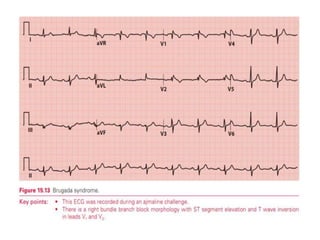
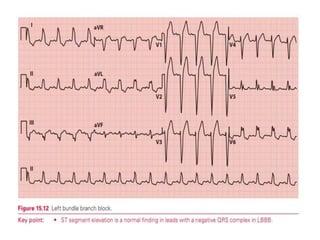
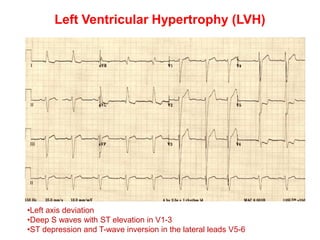
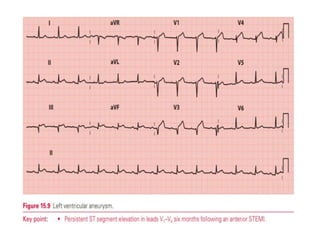
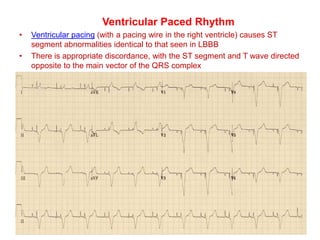
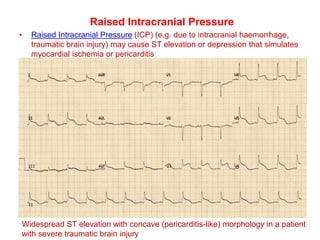
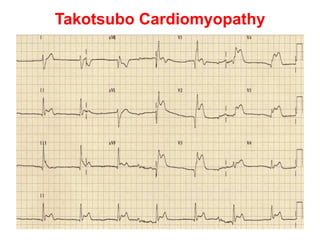
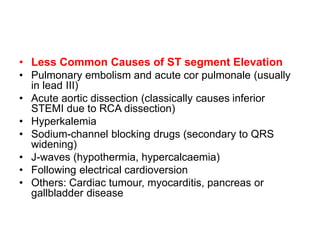
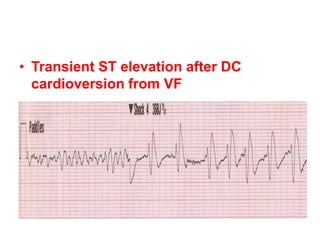
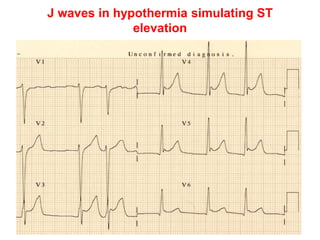
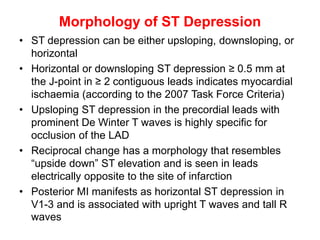
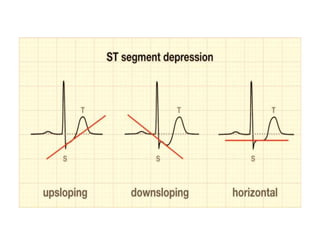
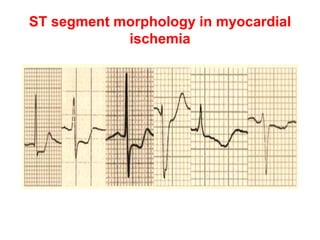
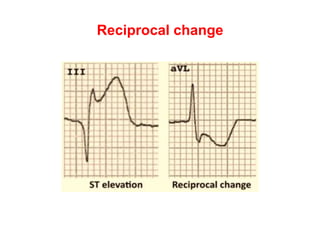
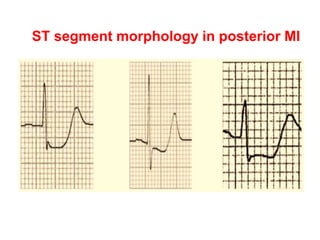
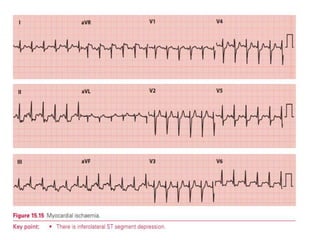
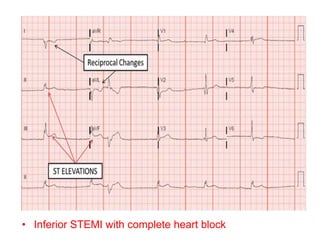
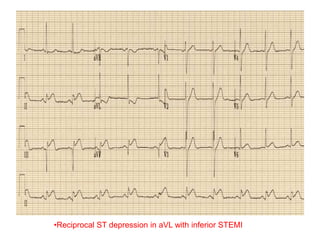
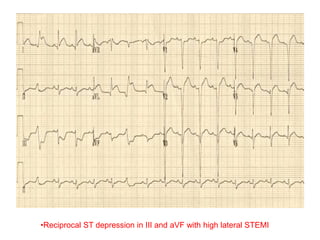
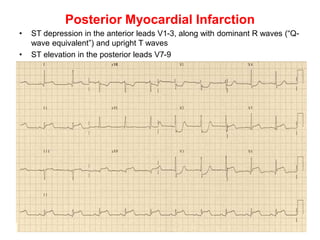
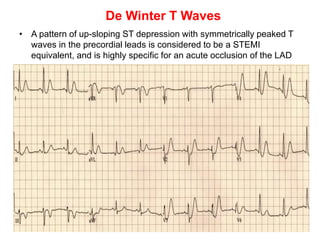
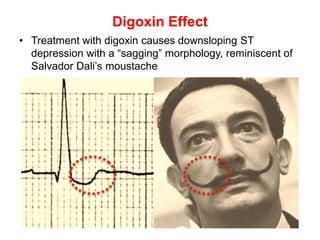
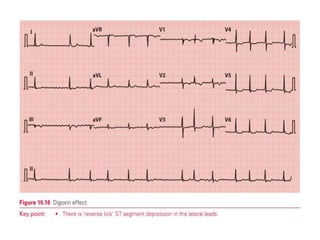
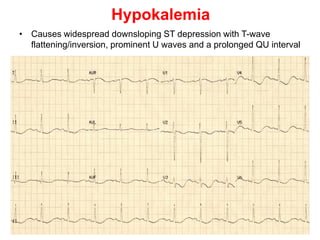
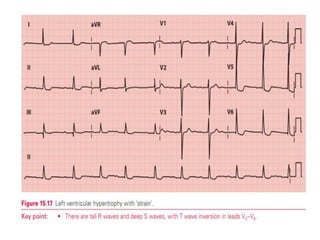
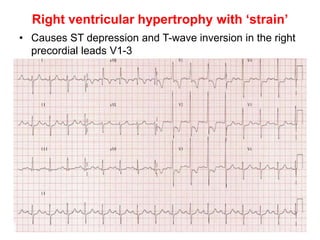
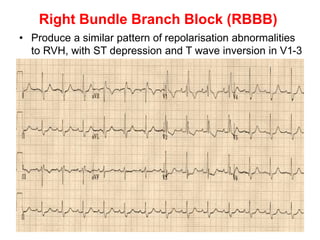
The document discusses the ST segment of the ECG and various abnormalities that can occur. It notes that the ST segment represents the interval between ventricular depolarization and repolarization. ST segment elevation or depression can indicate myocardial ischemia or infarction. Various conditions are described that can cause ST segment changes, including myocardial infarction in different coronary artery territories, coronary vasospasm, pericarditis, early repolarization, and others. The morphology and patterns of ST segment abnormalities are discussed for evaluating these conditions.