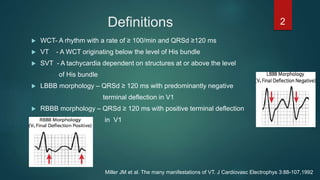
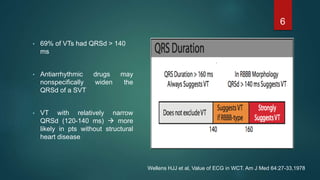
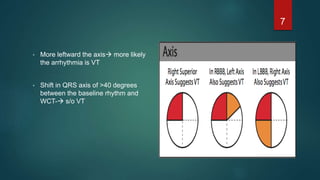
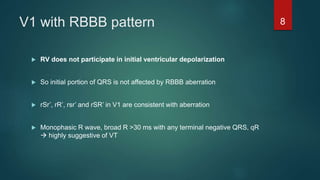
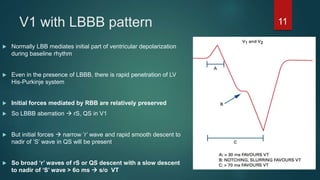
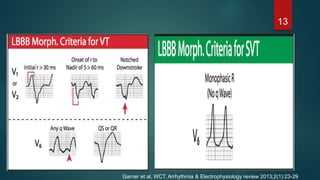
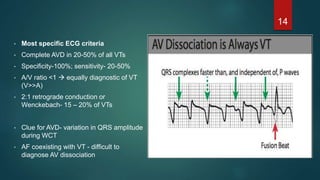
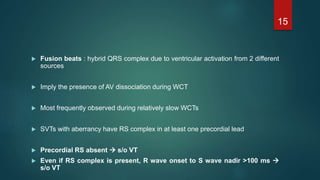
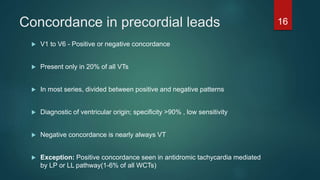
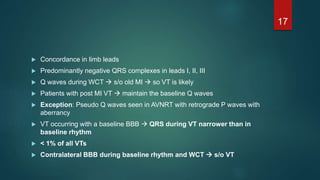
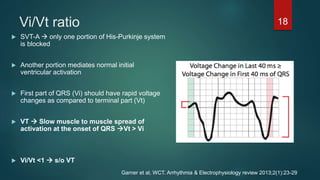
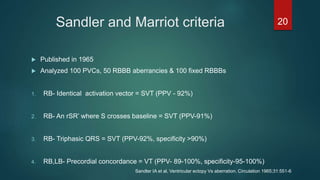
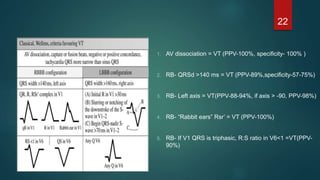
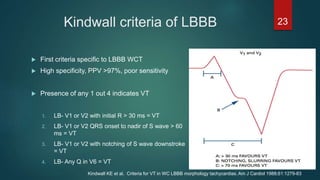
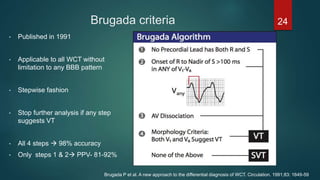
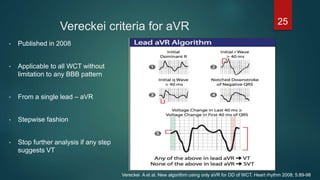
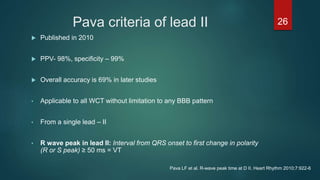
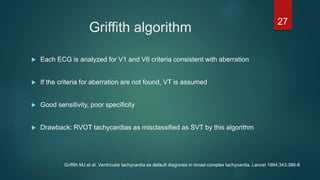
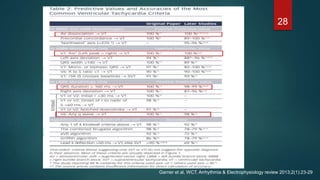
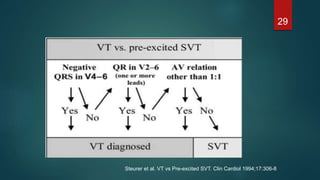
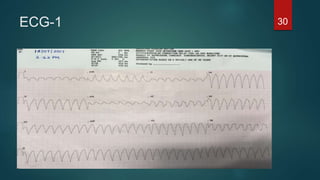
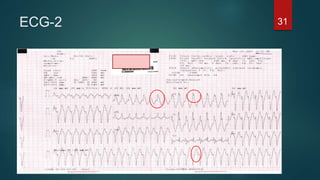
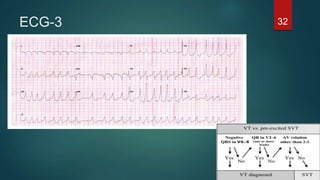
The document discusses wide complex tachycardia (WCT), focusing on differentiating between ventricular tachycardia (VT) and supraventricular tachycardia (SVT). It provides criteria for diagnosis based on ECG morphology, patient history, and specific characteristics related to conduction abnormalities. Accurate diagnosis is crucial to avoid mismanagement, as treatment for VT differs significantly from that for SVT.