1. The document provides guidelines on the diagnosis and management of diabetes and prediabetes from the American Diabetes Association. It discusses classification of diabetes, diagnostic criteria, screening recommendations, prevention of type 2 diabetes, glycemic targets, and management of complications.
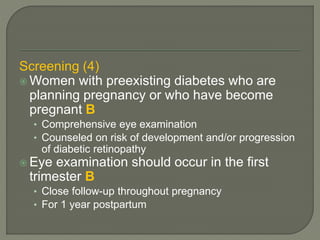
2. Testing and screening recommendations are provided for both types of diabetes as well as gestational diabetes. Lifestyle and medical interventions are recommended for preventing or delaying type 2 diabetes in those with prediabetes.
3. The guidelines cover medical nutrition therapy, diabetes self-management education, physical activity, hypoglycemia management, and immunization for patients with diabetes. Control of cardiovascular risk factors is emphasized for preventing diabetes complications.