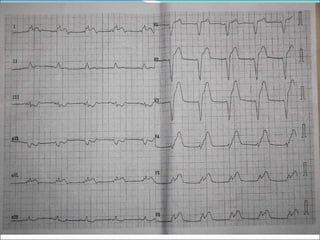
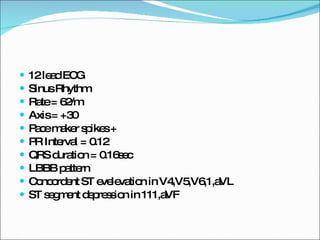
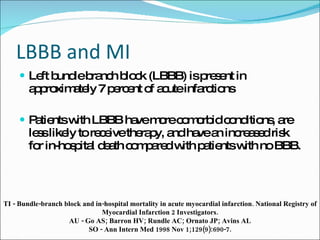
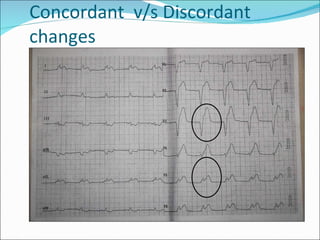
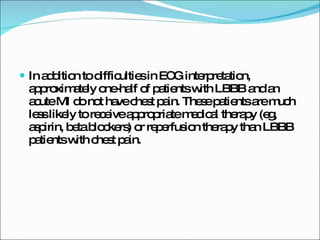
1. The document discusses electrocardiogram (ECG) findings in a patient presenting with left bundle branch block (LBBB) and possible myocardial infarction (MI).
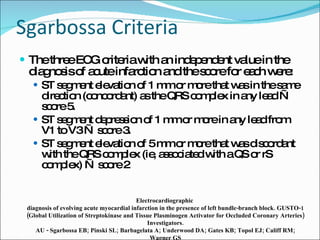
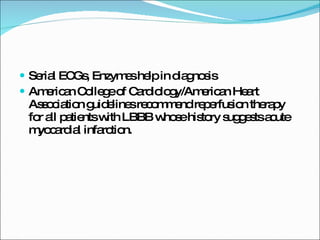
2. It outlines criteria developed by Sgarbossa et al. that can help diagnose MI in the presence of LBBB, with a Sgarbossa score of 3 or more being highly specific.
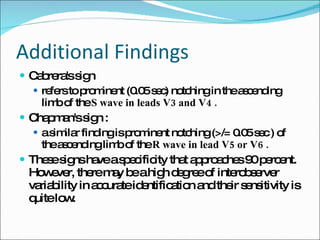
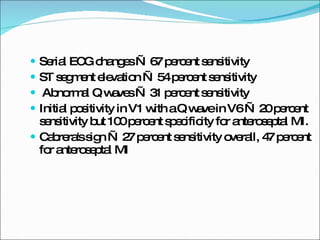
3. Additional ECG signs mentioned that suggest underlying MI in LBBB include deep T wave inversions, QR complexes, Cabrera's sign, and Chapman's sign. However, these have low sensitivity and interpretation can vary.