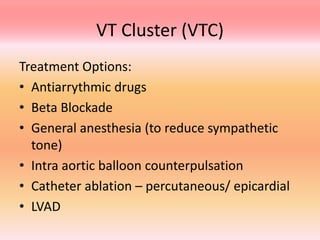
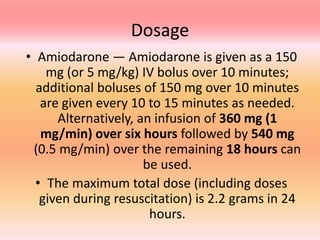
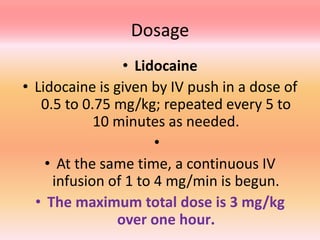
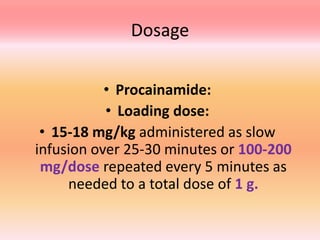
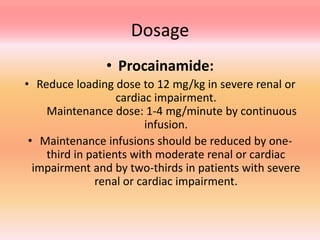
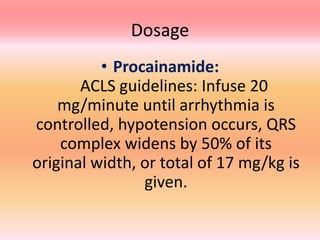
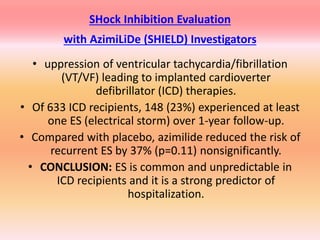
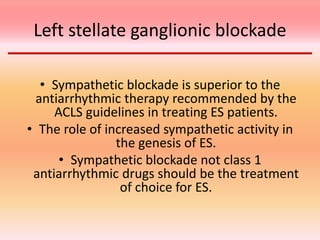
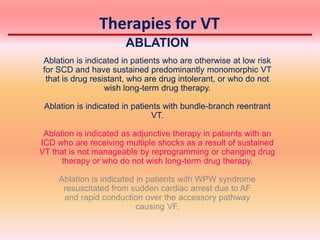
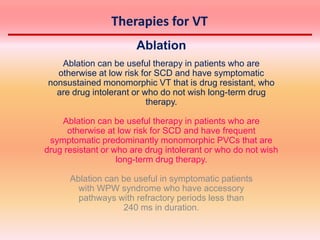
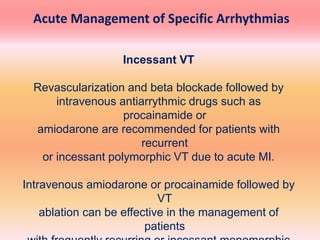
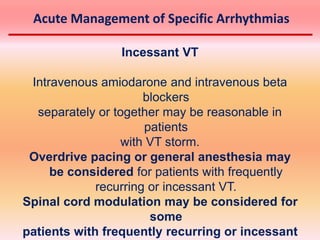
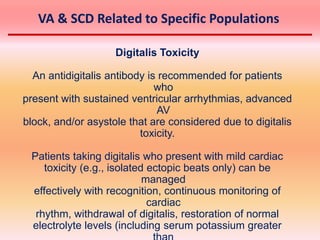
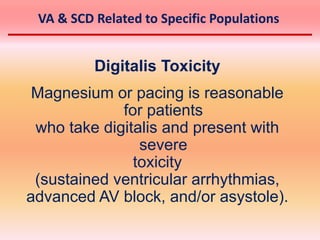
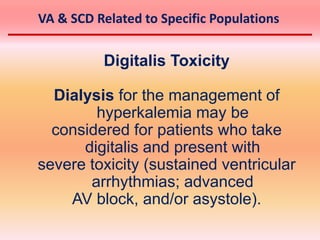
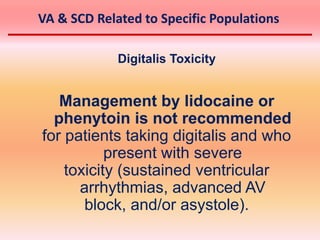
This document discusses ventricular tachycardia (VT) clusters and incessant VT. It defines a VT cluster as 3 or more sustained VTs within 24 hours. Treatment options discussed include antiarrhythmic drugs, ablation, anesthesia, and LVAD. Amiodarone, lidocaine, and procainamide dosages are provided. Left stellate ganglion blockade is suggested as superior to antiarrhythmic drugs for electrical storms. The document also discusses therapies for VT including ablation and digitalis toxicity management.