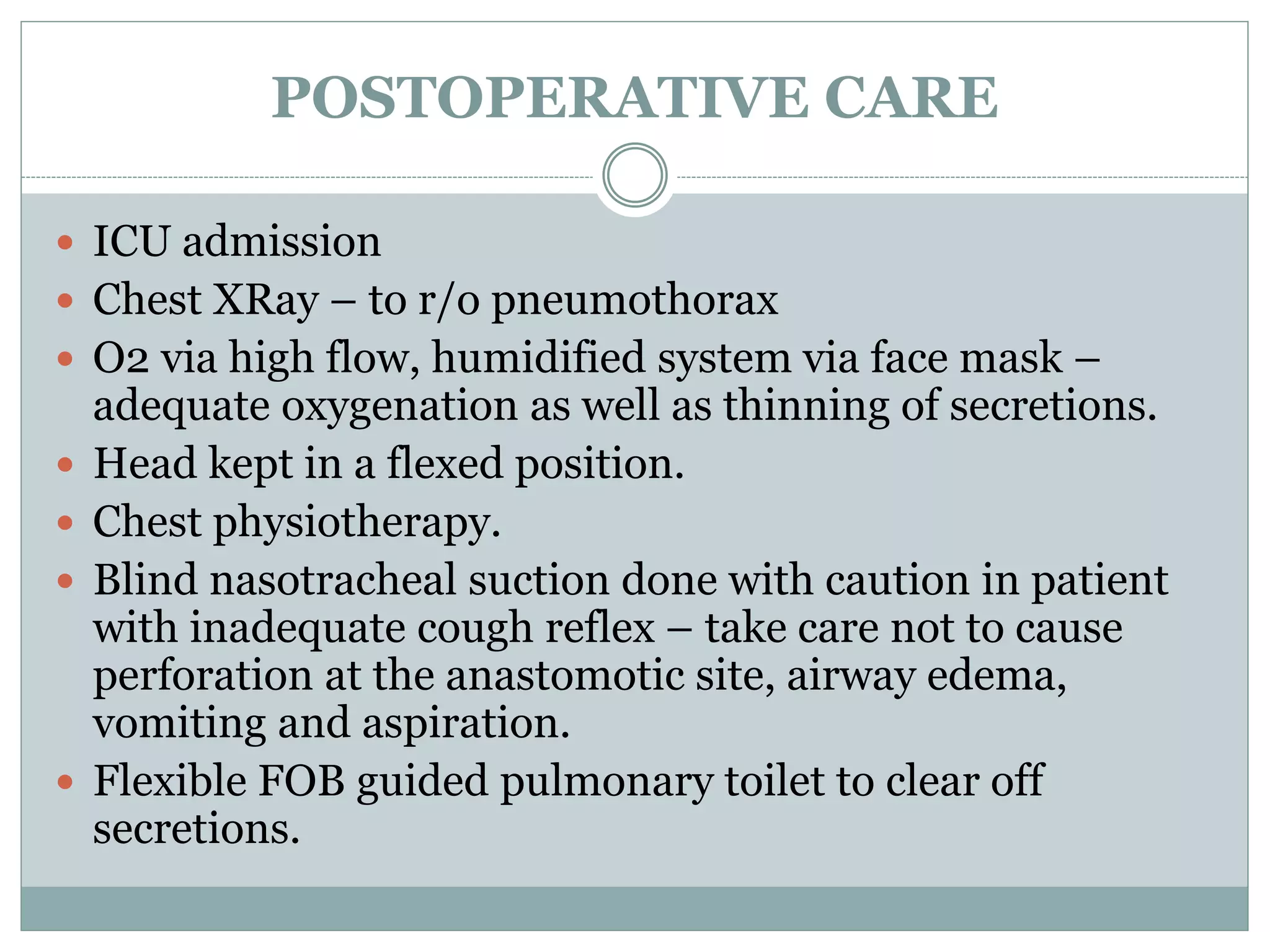
The document discusses the preoperative evaluation, anesthetic management considerations, and postoperative care for patients undergoing tracheal resection surgery. It covers topics like evaluating the airway, planning induction and intubation, positioning for different types of tracheal lesions, intraoperative ventilation techniques, and managing complications in the postoperative period. Tracheal resection surgery requires careful planning and execution of anesthesia to maintain adequate ventilation and oxygenation given the risks of airway obstruction.