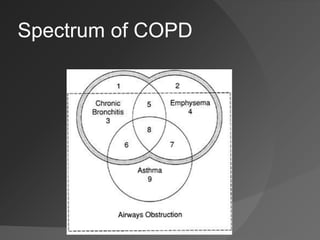
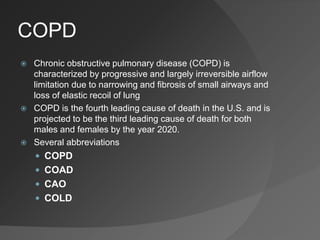
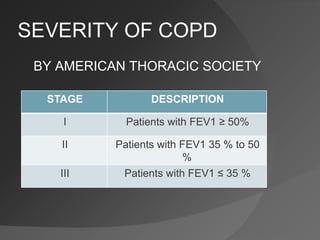
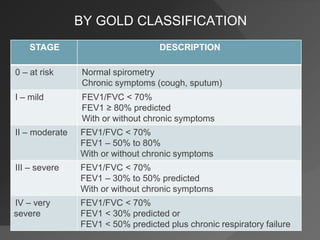
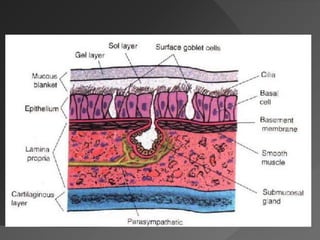
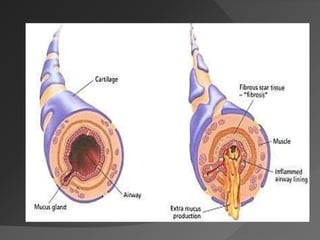
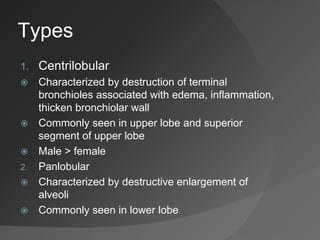
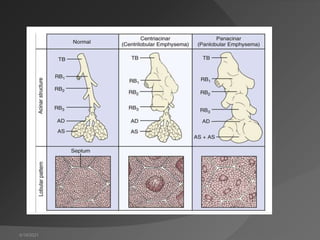
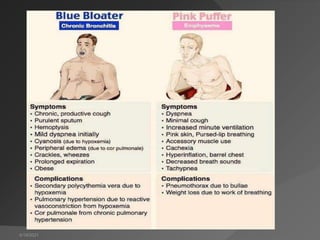
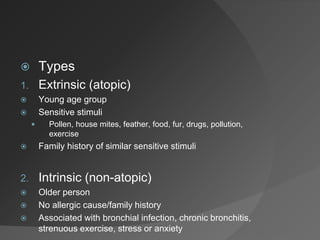
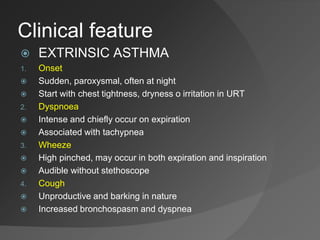
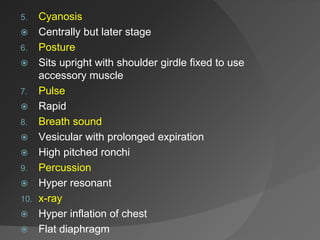
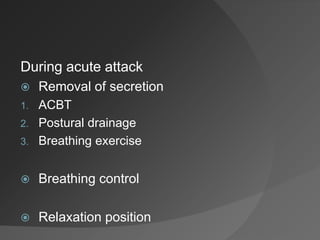
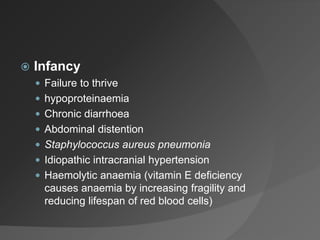
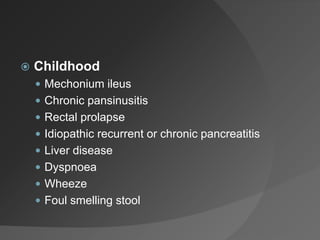
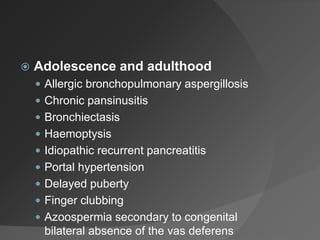
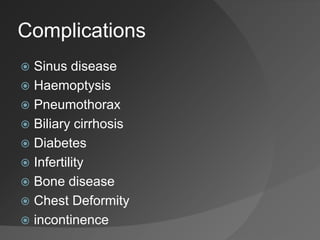
The document discusses various respiratory disorders, focusing on chronic obstructive pulmonary disease (COPD), chronic bronchitis, emphysema, asthma, bronchiectasis, and cystic fibrosis. It outlines the classification, causes, clinical features, and management of these conditions, highlighting their impact on airflow and lung function. Key treatment strategies include bronchodilators, steroids, physiotherapy, and methods to clear secretions.