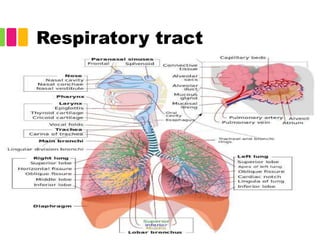
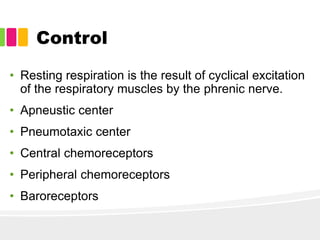
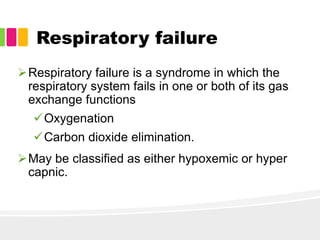
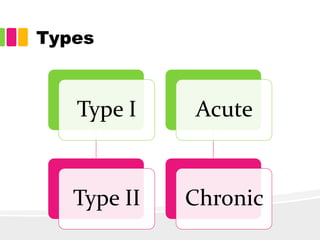
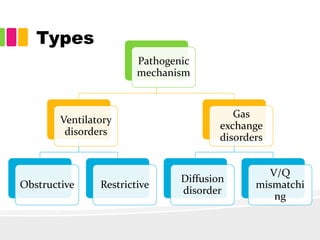
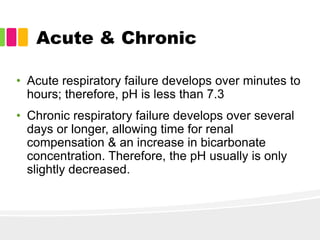
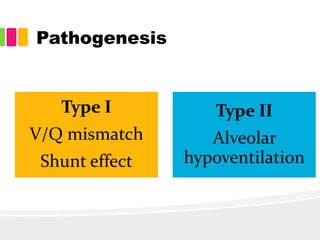
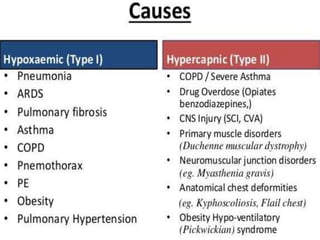
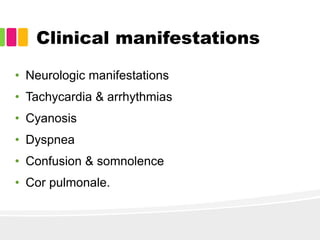
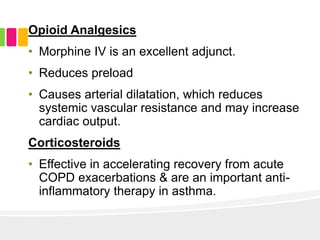
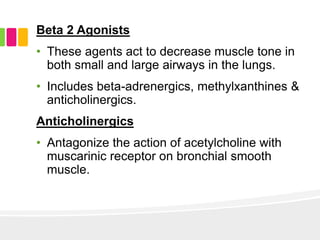
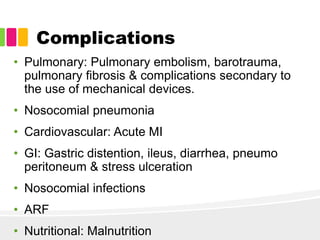
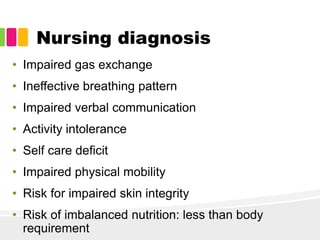
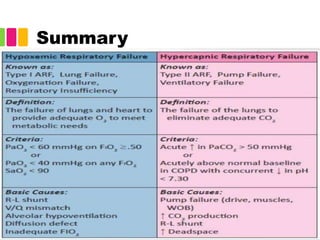
This document discusses respiratory failure, including its definition, types, causes, clinical manifestations, diagnostic evaluations, management, and complications. Respiratory failure is when the respiratory system fails to adequately oxygenate the blood or eliminate carbon dioxide. It can be classified as hypoxemic or hypercapnic. Acute respiratory failure develops rapidly over hours while chronic develops over days. Management involves treating the underlying cause, providing oxygen supplementation, monitoring vital signs, and supporting respiratory function. Complications can affect the lungs, heart, gastrointestinal system, and risk of infection.
![References
1. Hinkle LJ, Cheever HK. Brunner & Sudharth's textbook of
medical surgical nursing. 13th Edition. I volume .New
Delhi: Wolters Kluwer Publications; 2014.Pp 545-47
2. Respiratory Failure: Background, Pathophysiology,
Etiology [Internet]. [cited 2018 Mar 6]. Available from:
https://emedicine.medscape.com/article/167981-
overview#showall
3. Pathophysiology of acute respiratory failure. - PubMed -
NCBI [Internet]. [cited 2018 Mar 6]. Available from:
https://www.ncbi.nlm.nih.gov/pubmed/8200186
4. NCP Nursing Care Plan for Acute Respiratory Failure
[Internet]. [cited 2018 Mar 6]. Available from: http://nurse-
thought.blogspot.in/2011/03/ncp-nursing-care-plan-for-
acute_18.html](https://image.slidesharecdn.com/respiratoryfailure-180930134535/85/Respiratory-failure-23-320.jpg)
