1. Interstitial lung diseases (ILDs) involve the lung parenchyma including the alveoli, capillaries, and spaces between.
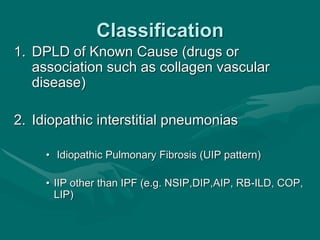
2. ILDs are classified based on known causes, idiopathic forms, and granulomatous types. Idiopathic pulmonary fibrosis is the most common idiopathic form.
3. Clinical presentation involves breathlessness, cough, and reduced lung function. Investigations include chest imaging showing infiltrates and fibrosis, and lung biopsies to determine classification. Treatment focuses on removing exposures, suppressing inflammation, and palliating symptoms primarily using corticosteroids.