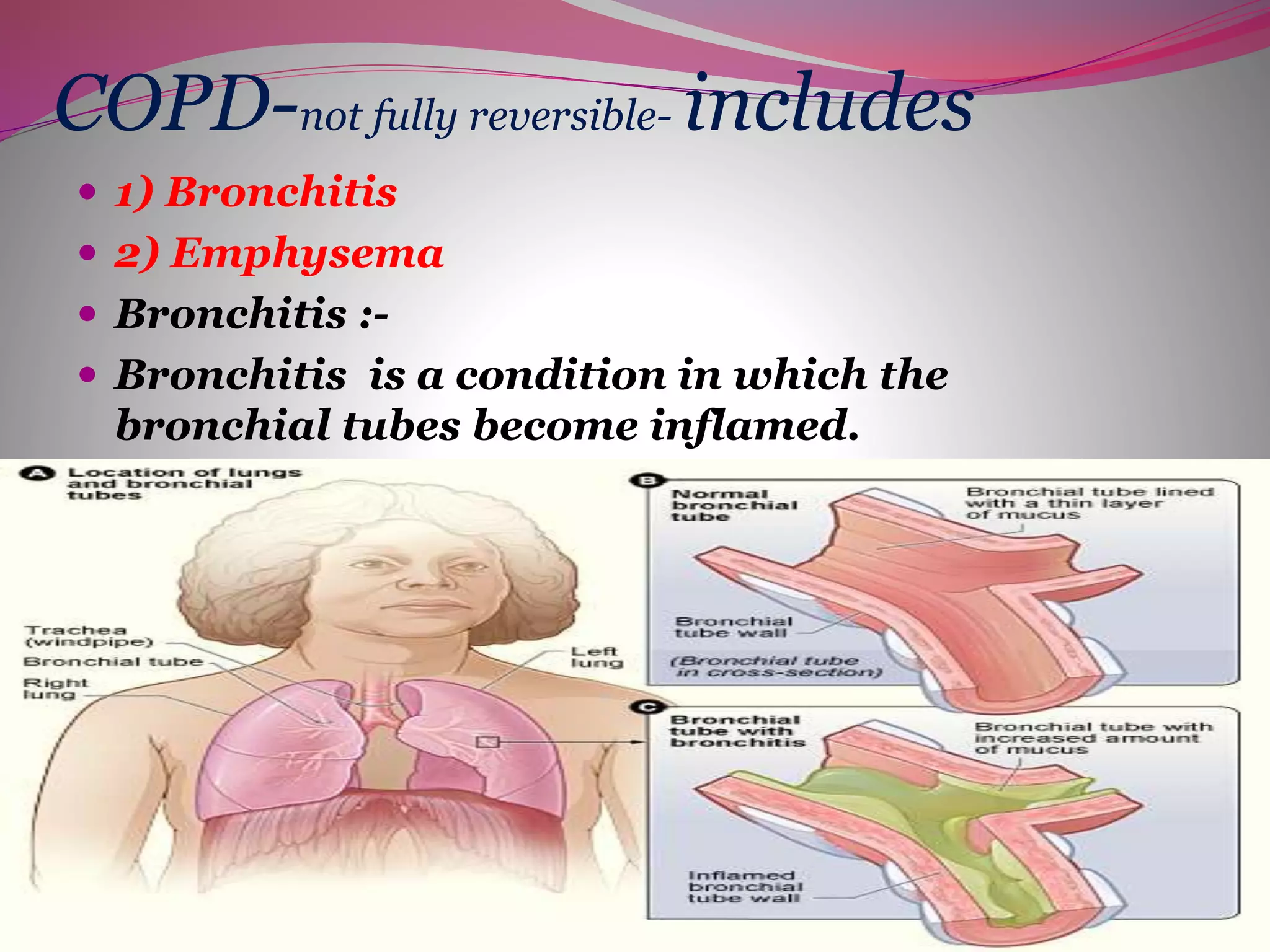
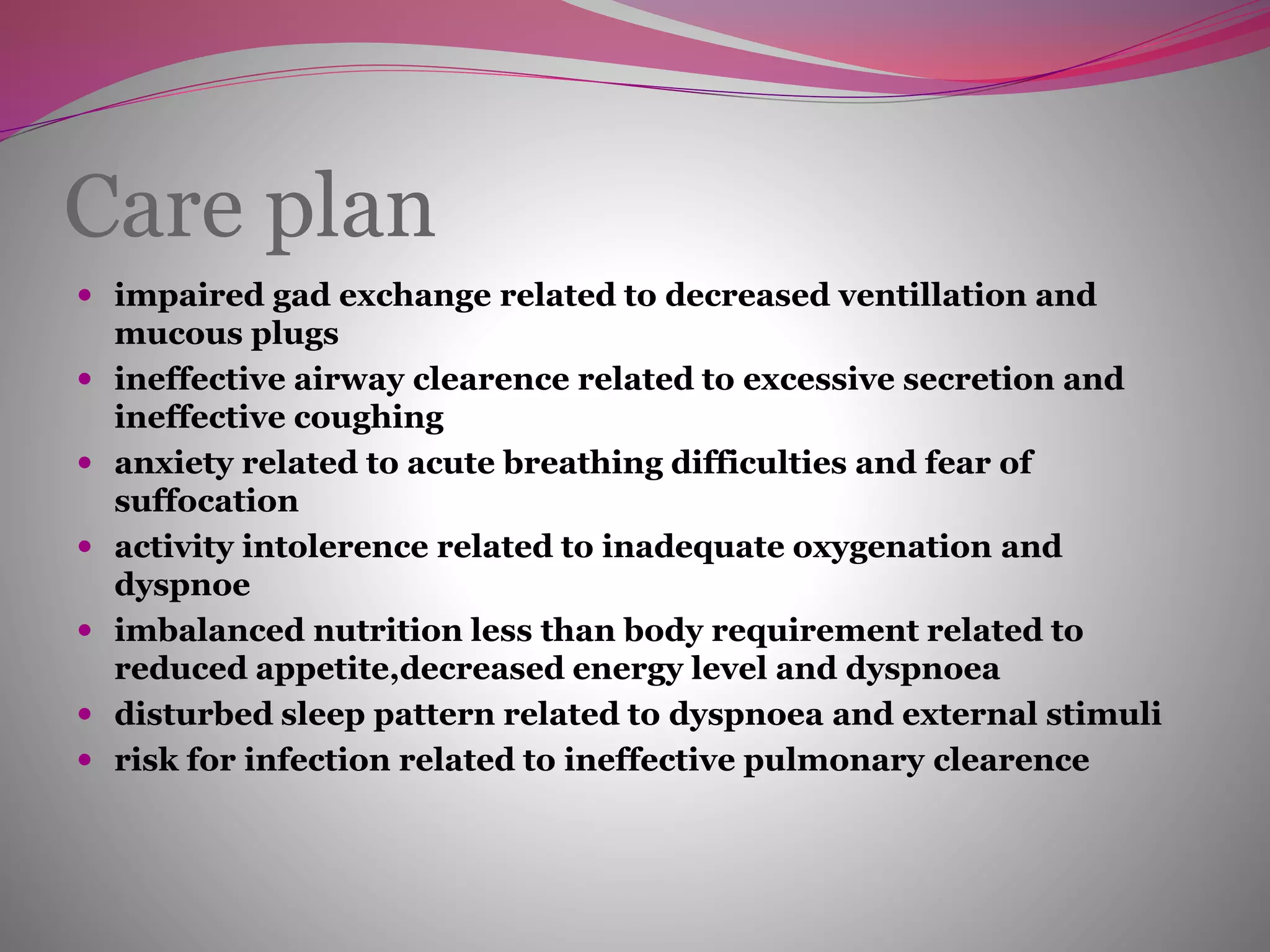
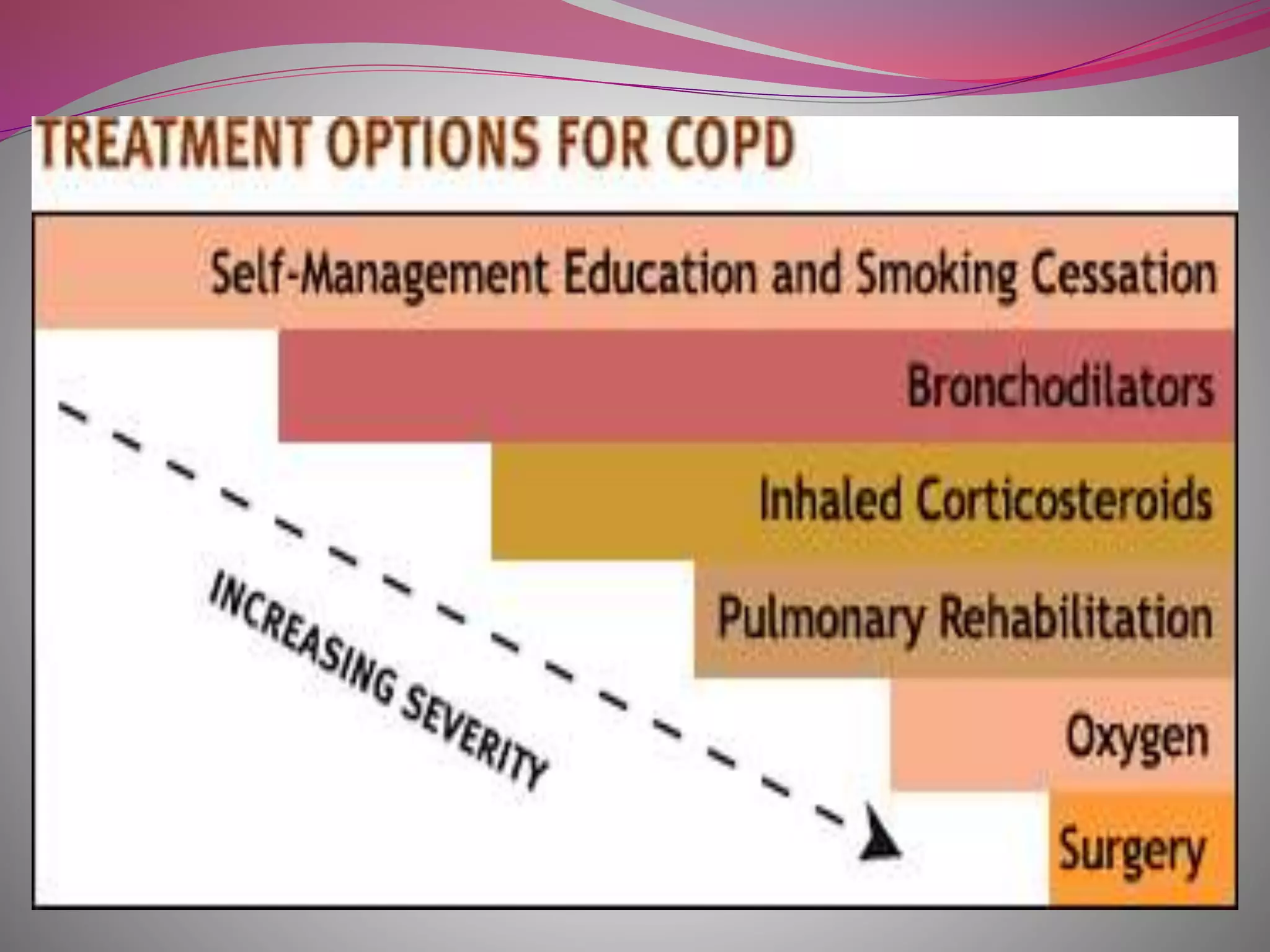
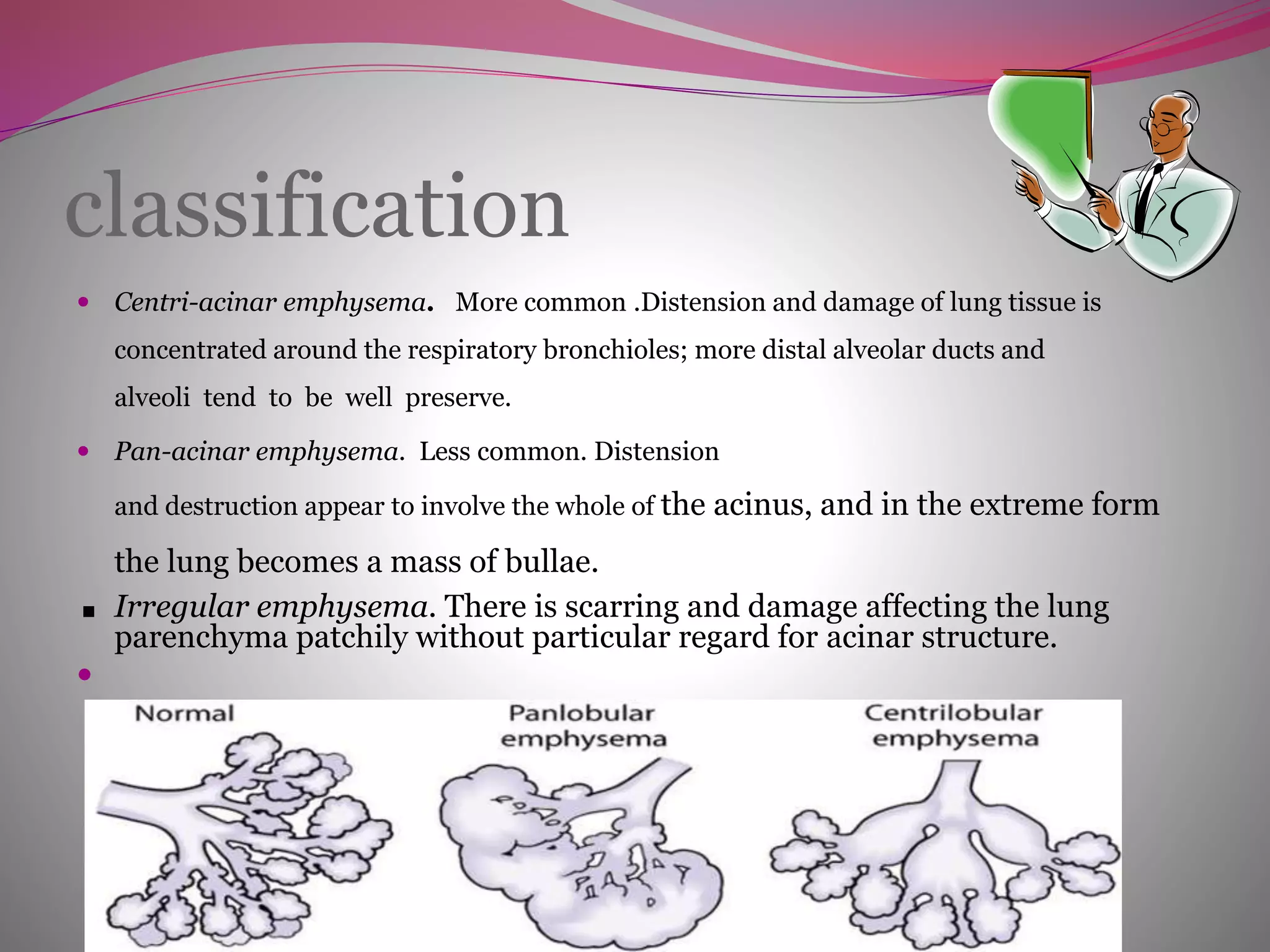
This document discusses obstructive pulmonary disorders including asthma and chronic obstructive pulmonary disease (COPD). It covers the causes of these conditions such as smoking, occupational exposures, air pollution, and genetics. The pathophysiology of COPD involves damage to airways and air sacs causing airflow limitation. Symptoms include coughing, wheezing and shortness of breath. Management involves medical treatment to improve ventilation, oxygen therapy, and surgery in some cases. Nursing care focuses on managing symptoms and preventing complications like infection.