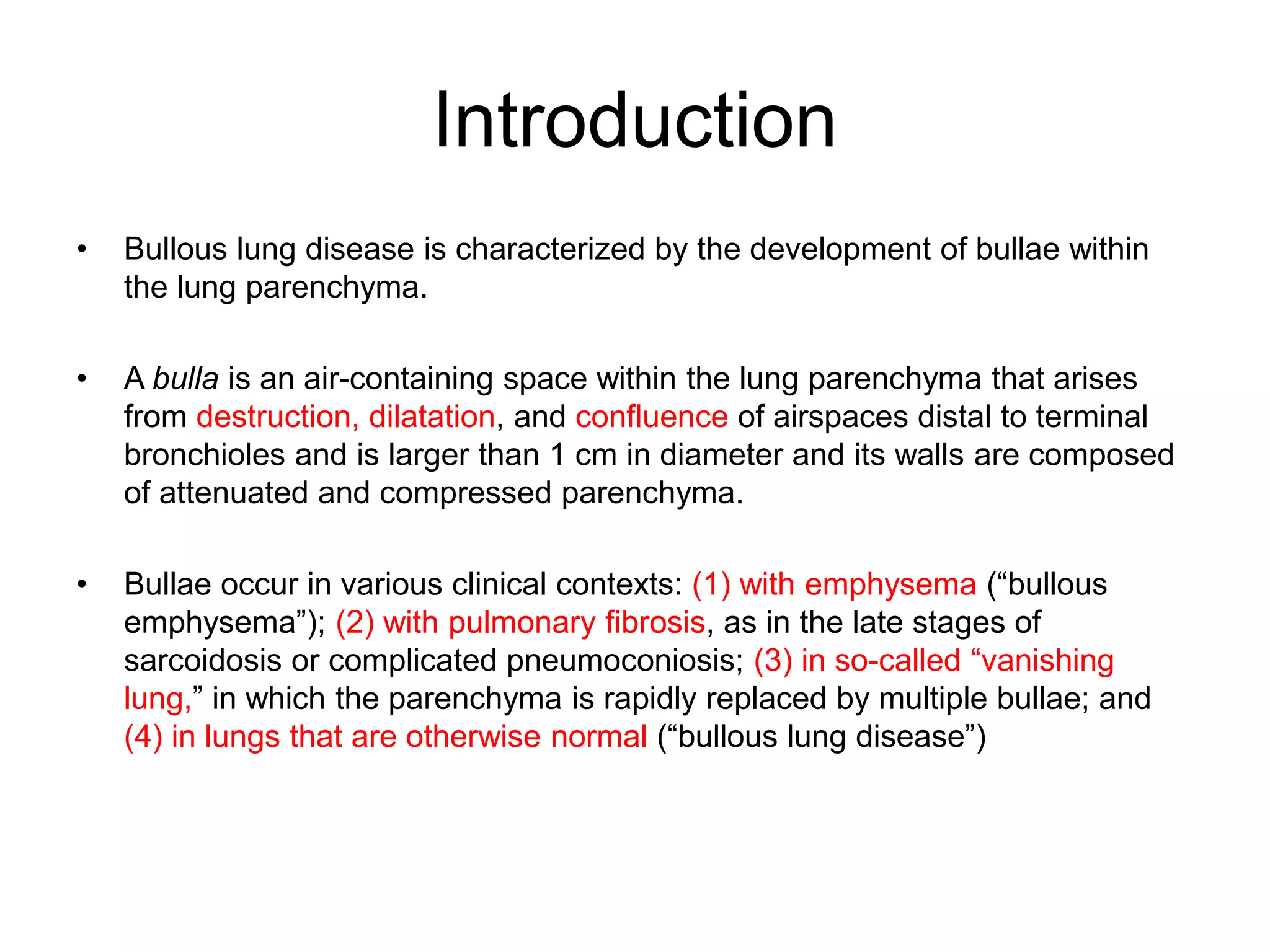
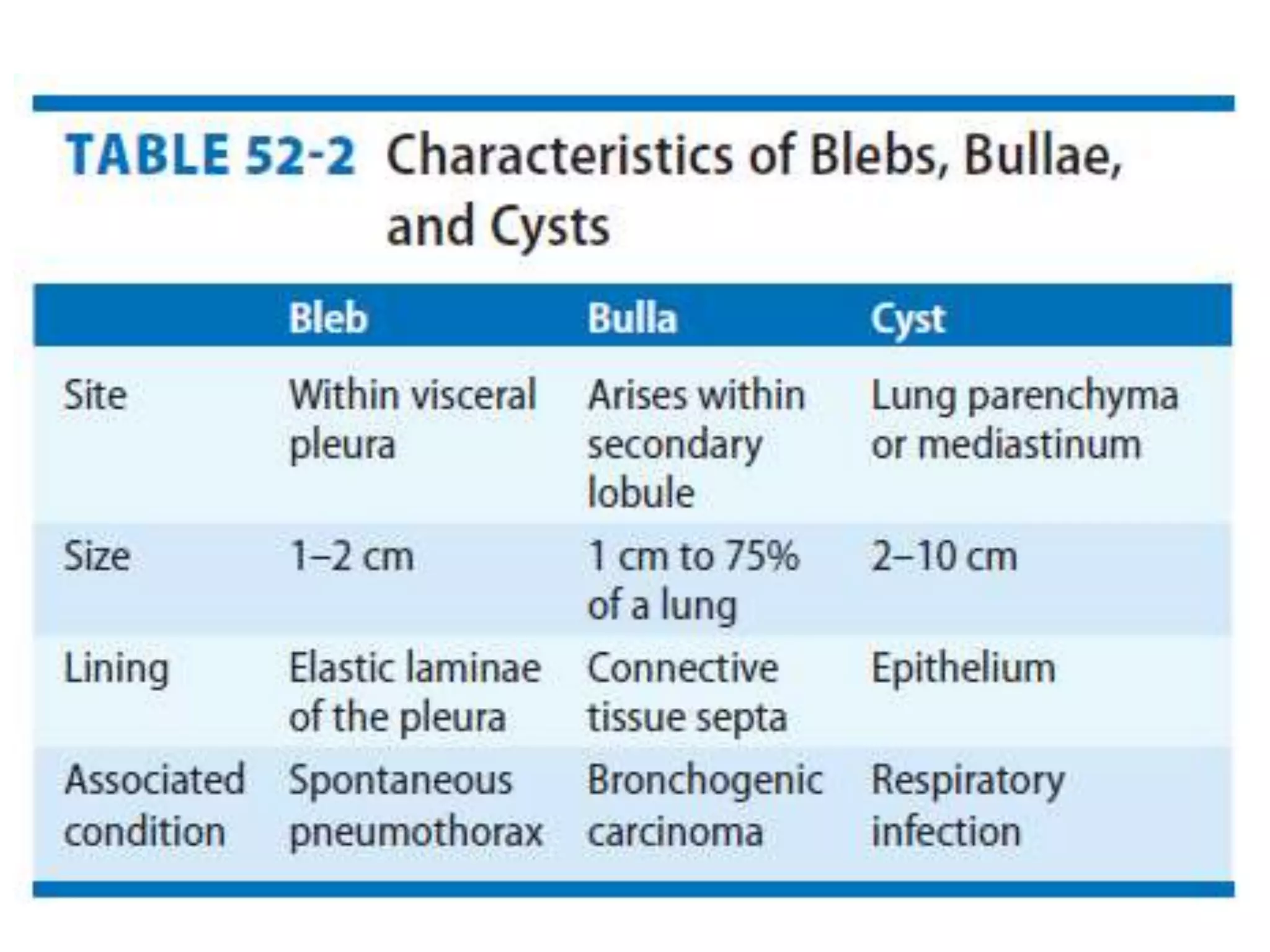
This document discusses the approach to bullous lung disease. It defines a bulla as a large air-containing space within the lung larger than 1 cm in diameter. Bullae can occur with emphysema, pulmonary fibrosis, or in otherwise normal lungs. HRCT is useful for evaluating the size, number and relationships of bullae. Pulmonary function testing may show obstructive lung disease, hyperinflation and reduced diffusion capacity. For surgical candidates, bullectomy or lung volume reduction surgery may be considered to treat symptoms or complications like spontaneous pneumothorax.