1) The document discusses preoperative evaluation and anesthetic considerations for thoracic surgery patients, with a focus on patients undergoing one-lung ventilation.
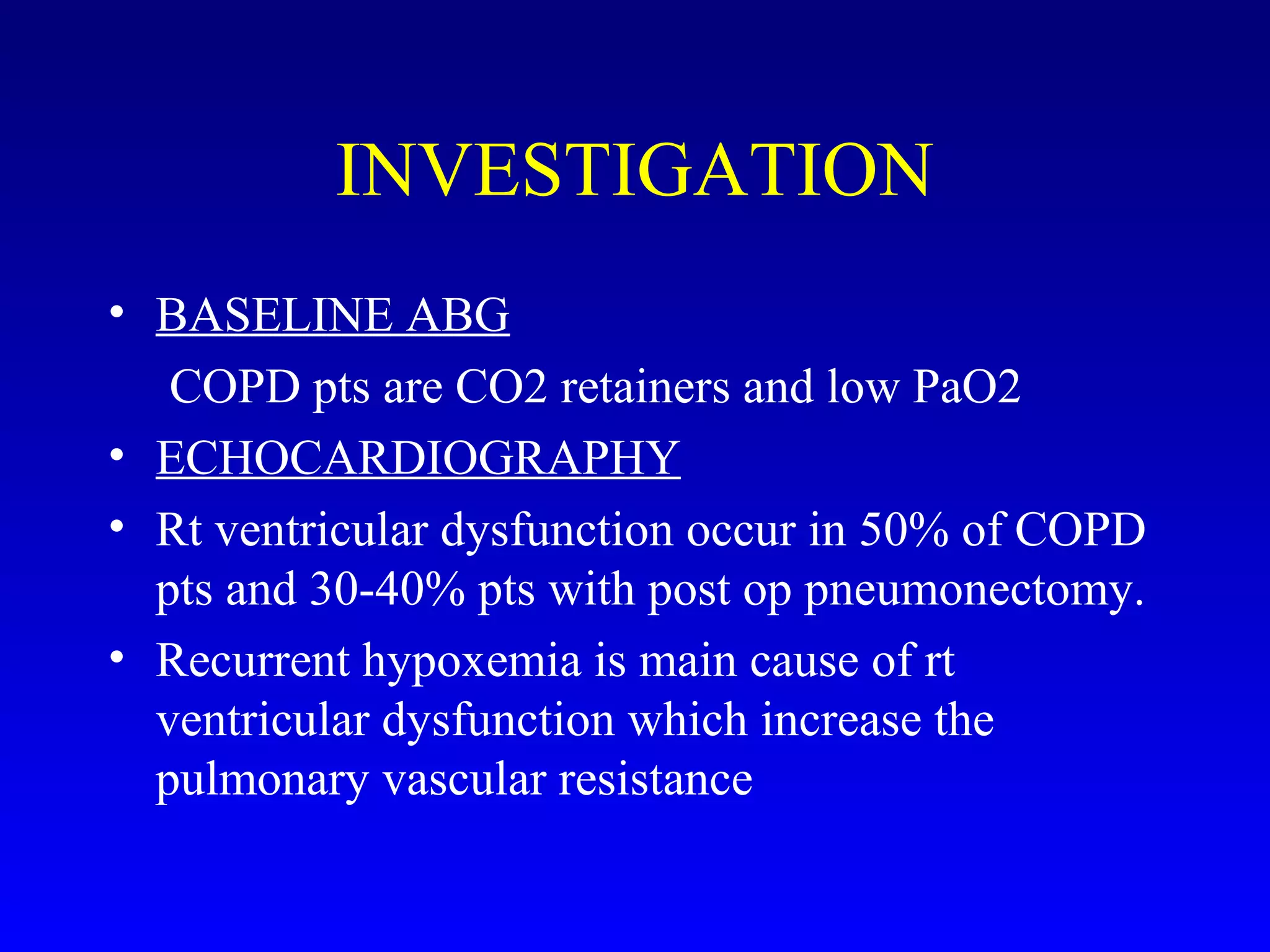
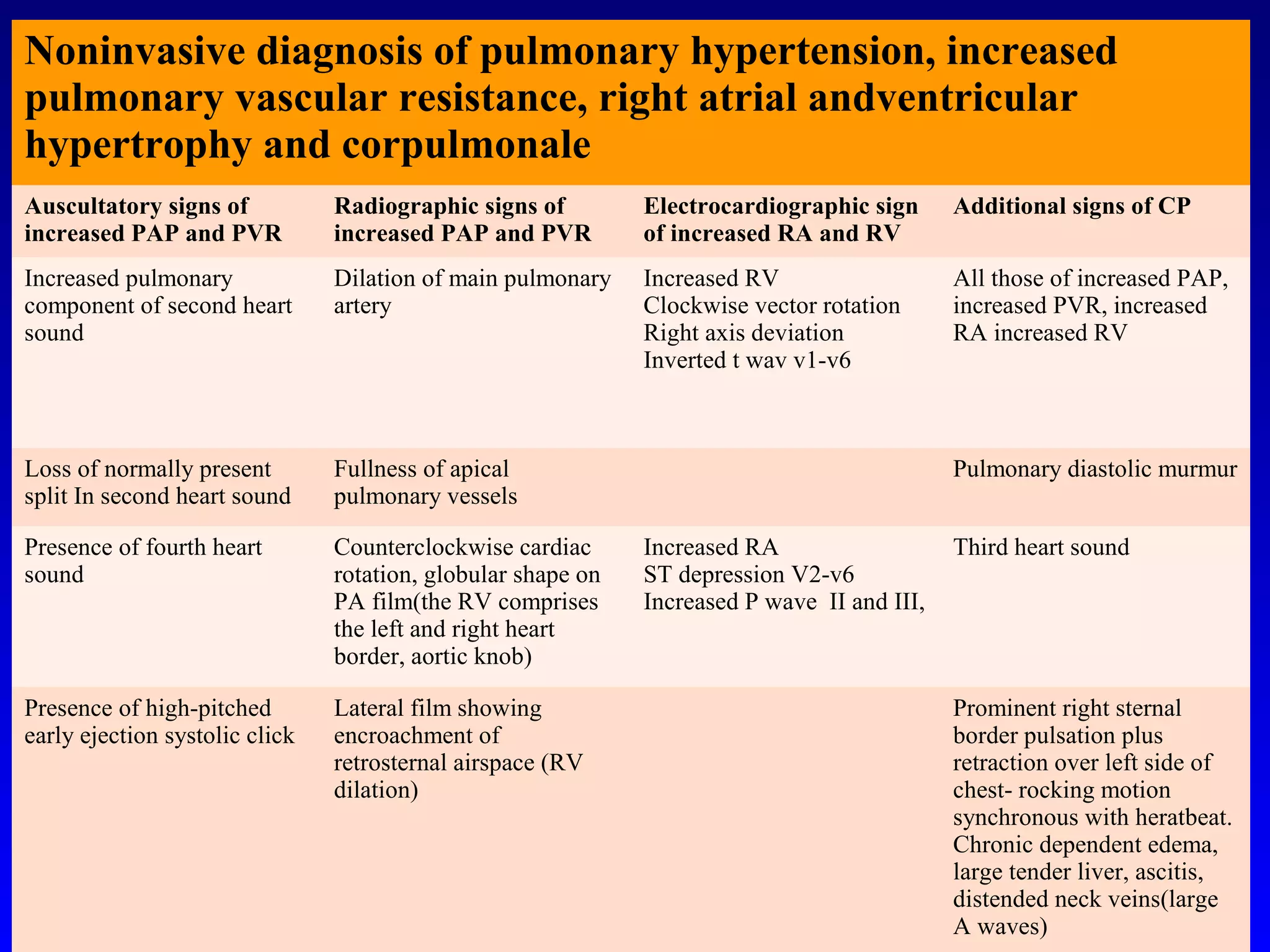
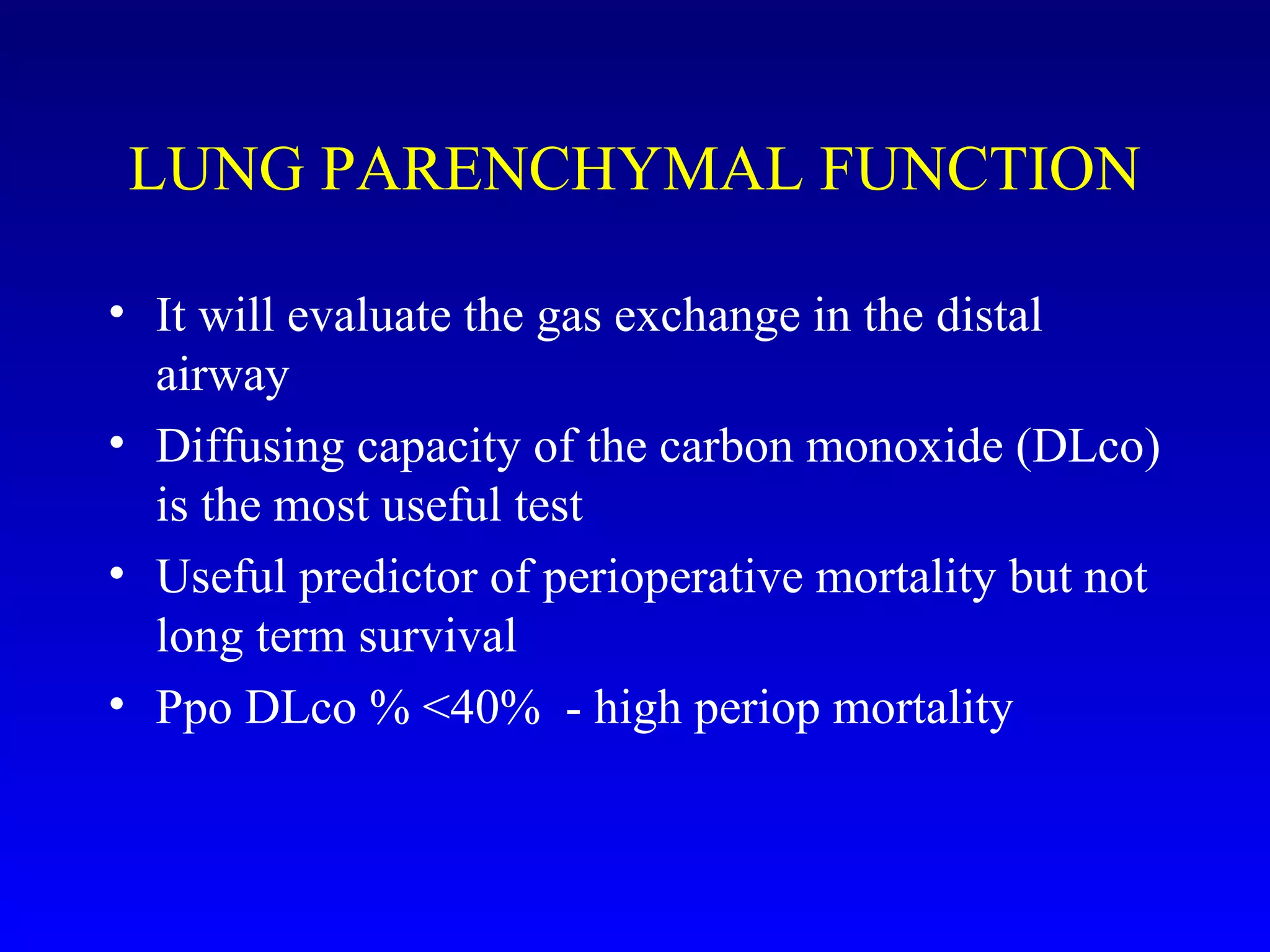
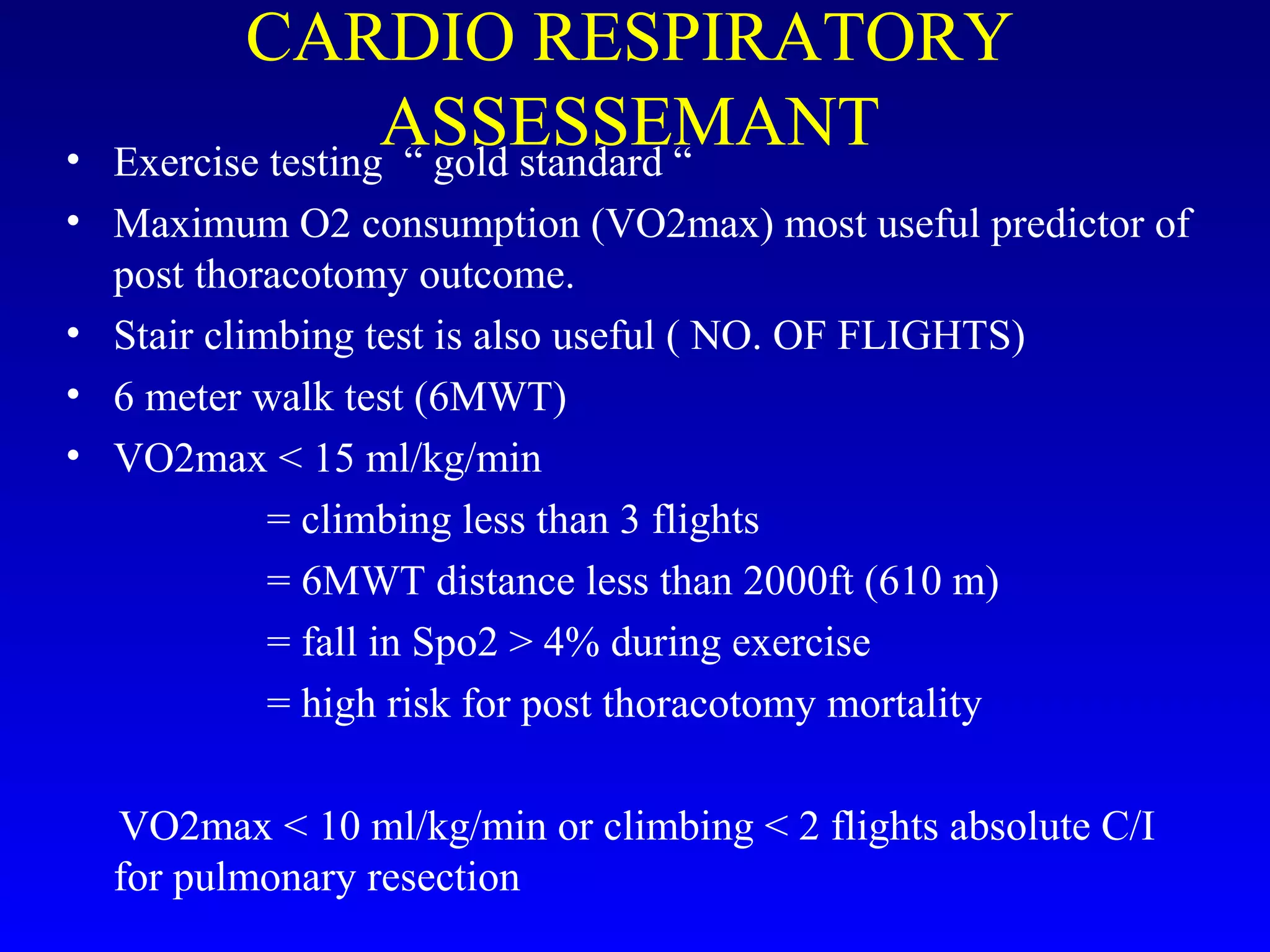
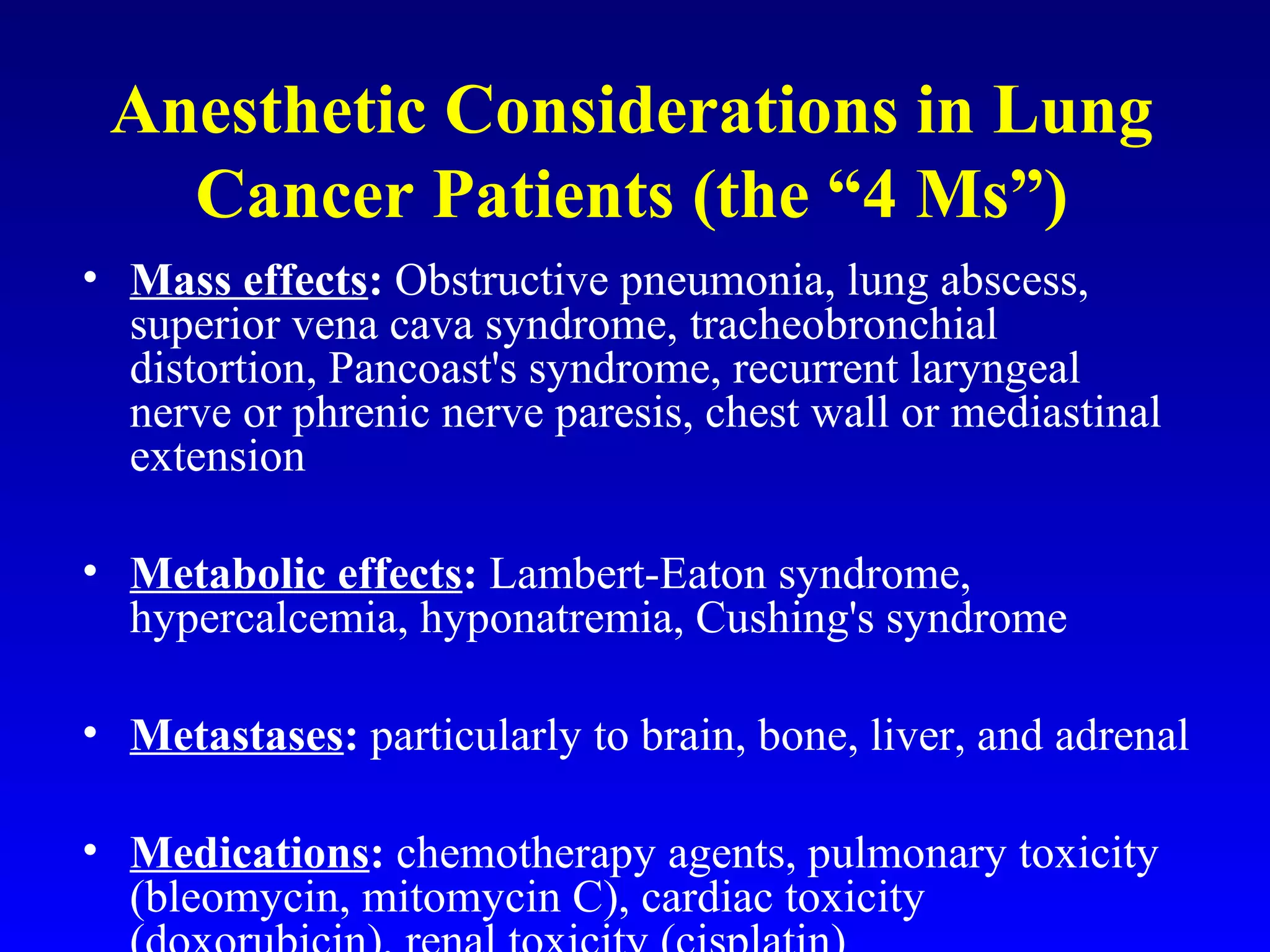
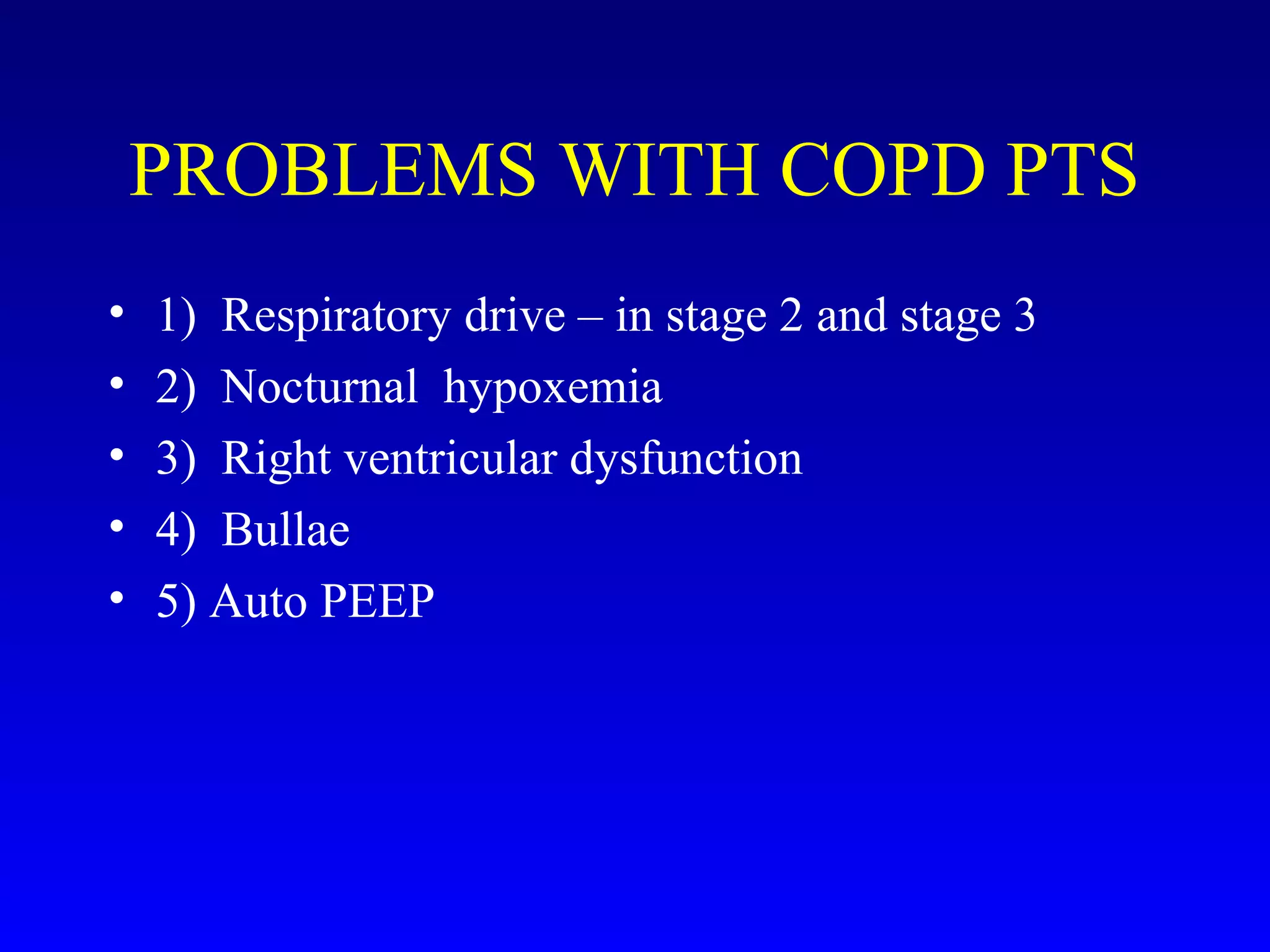
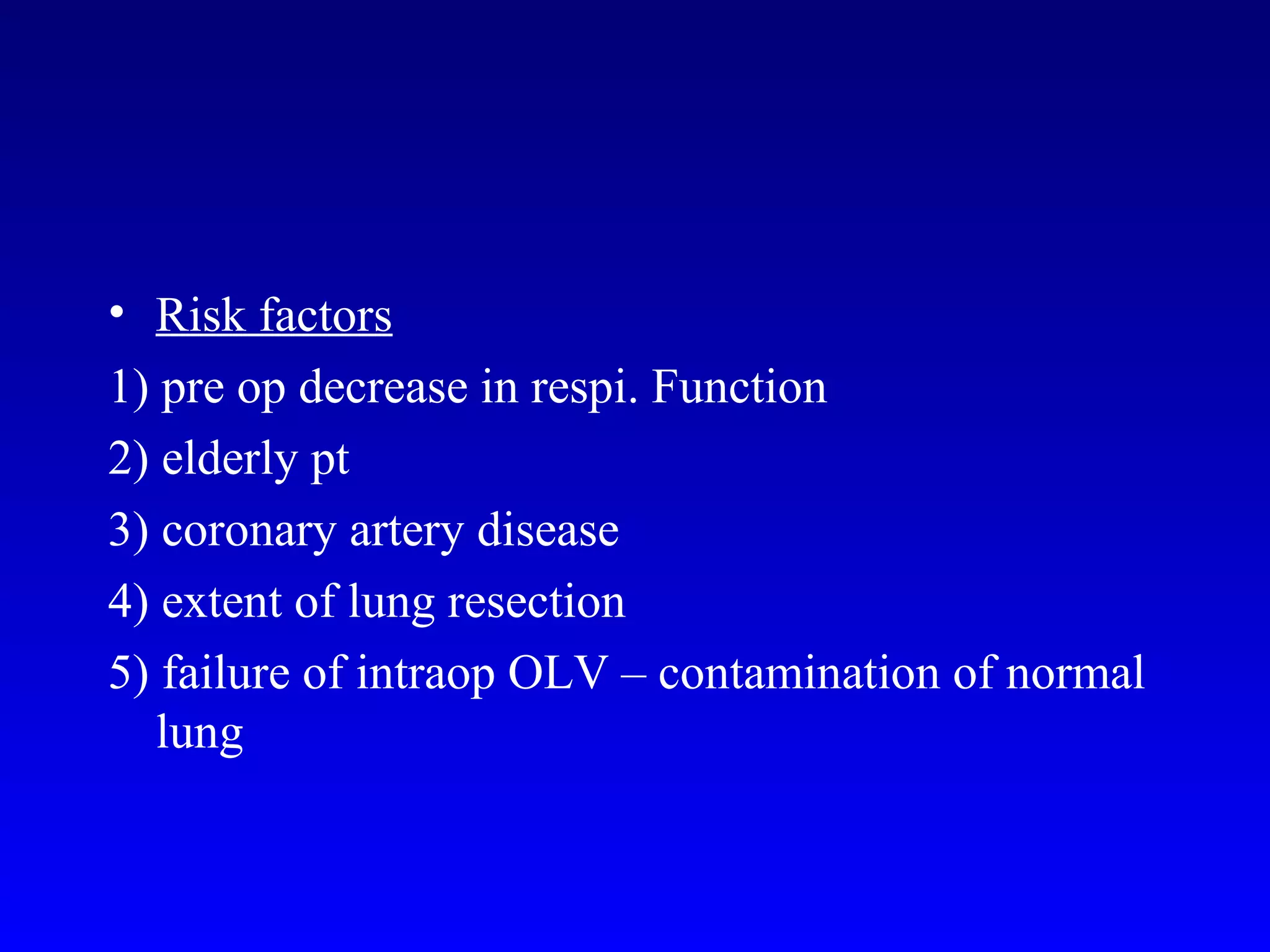
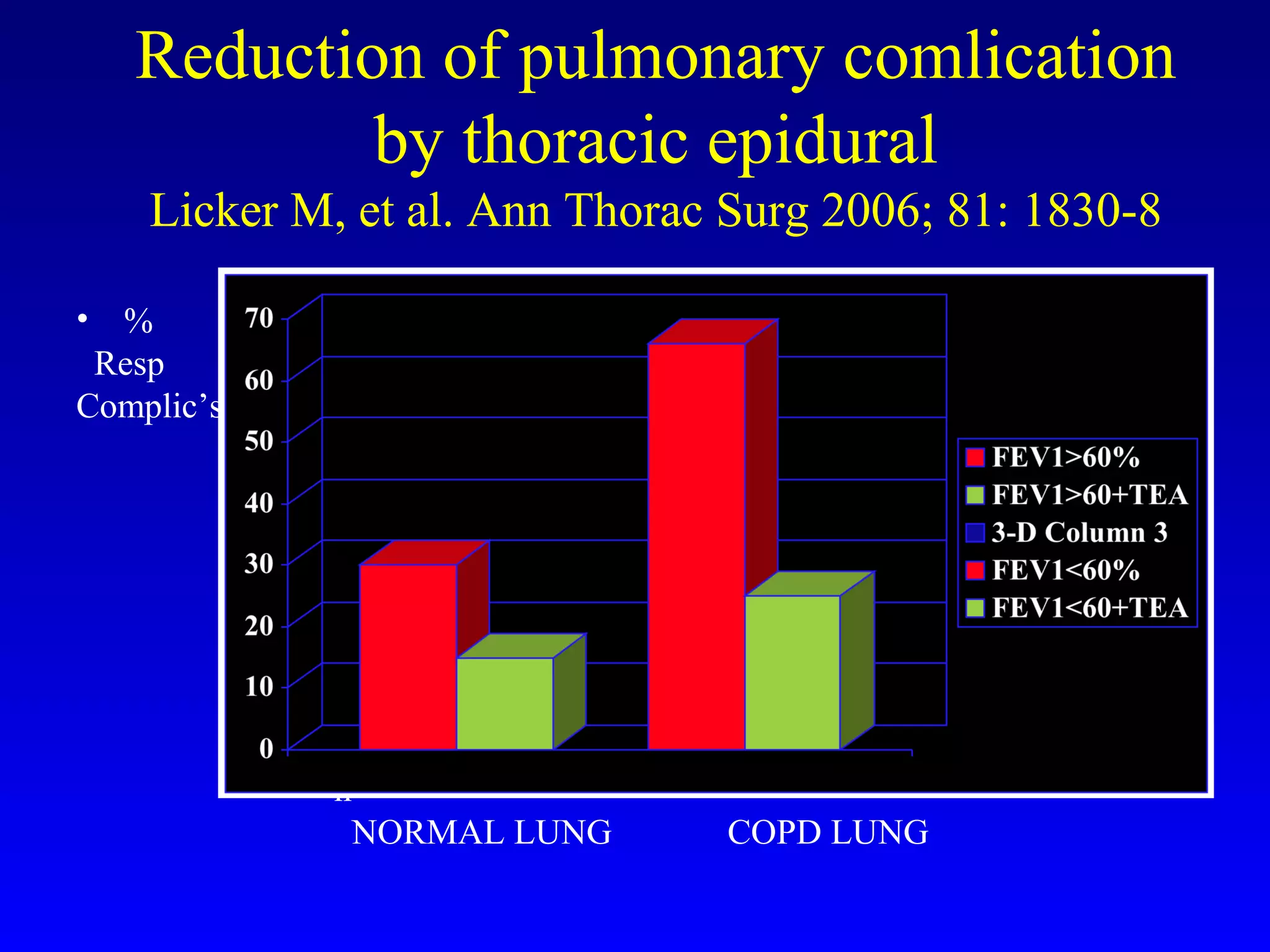
2) Key points of preoperative evaluation include assessing pulmonary function, cardiac status, investigating the extent of lung involvement, and optimizing patients with respiratory conditions like COPD.
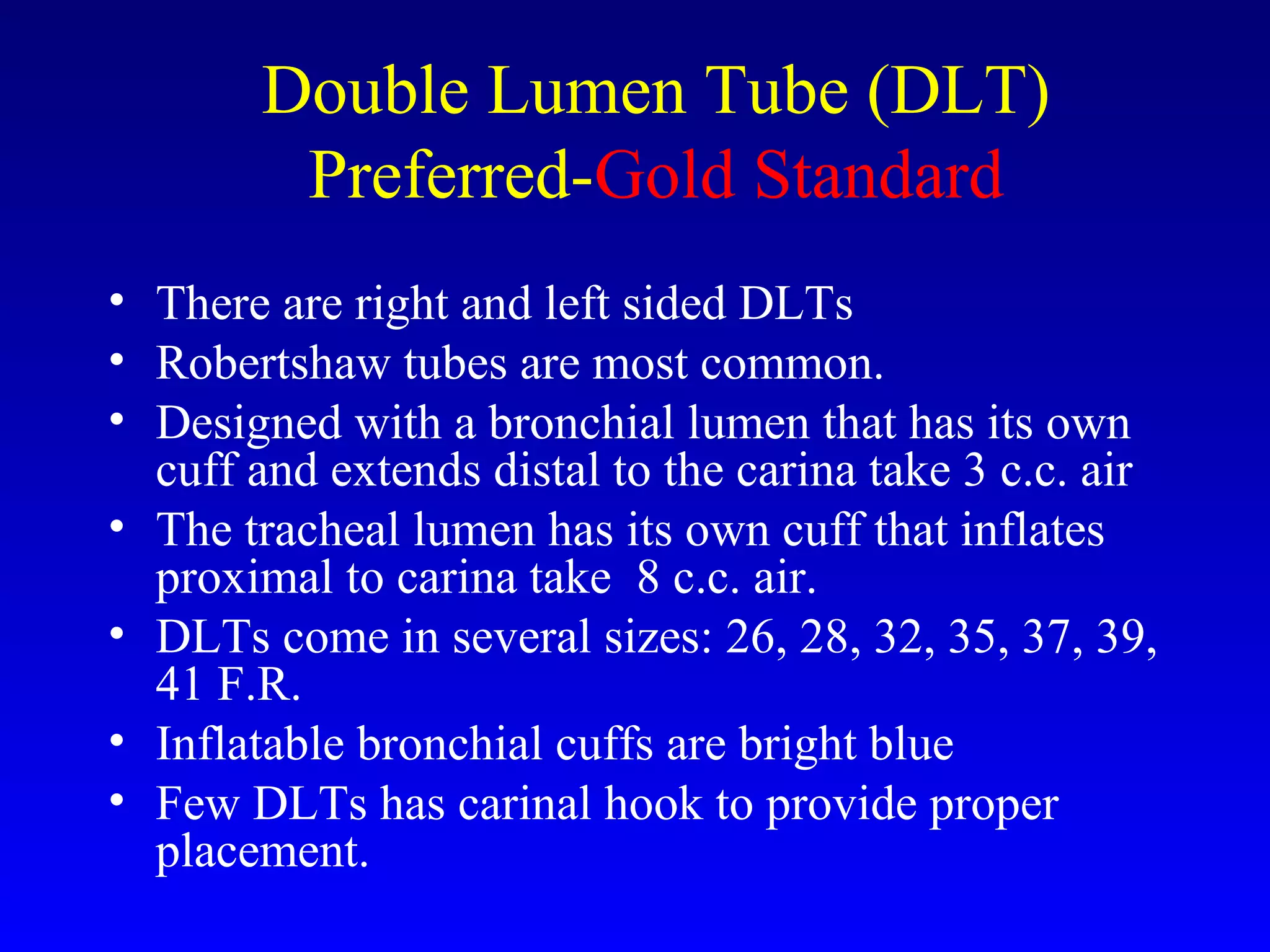
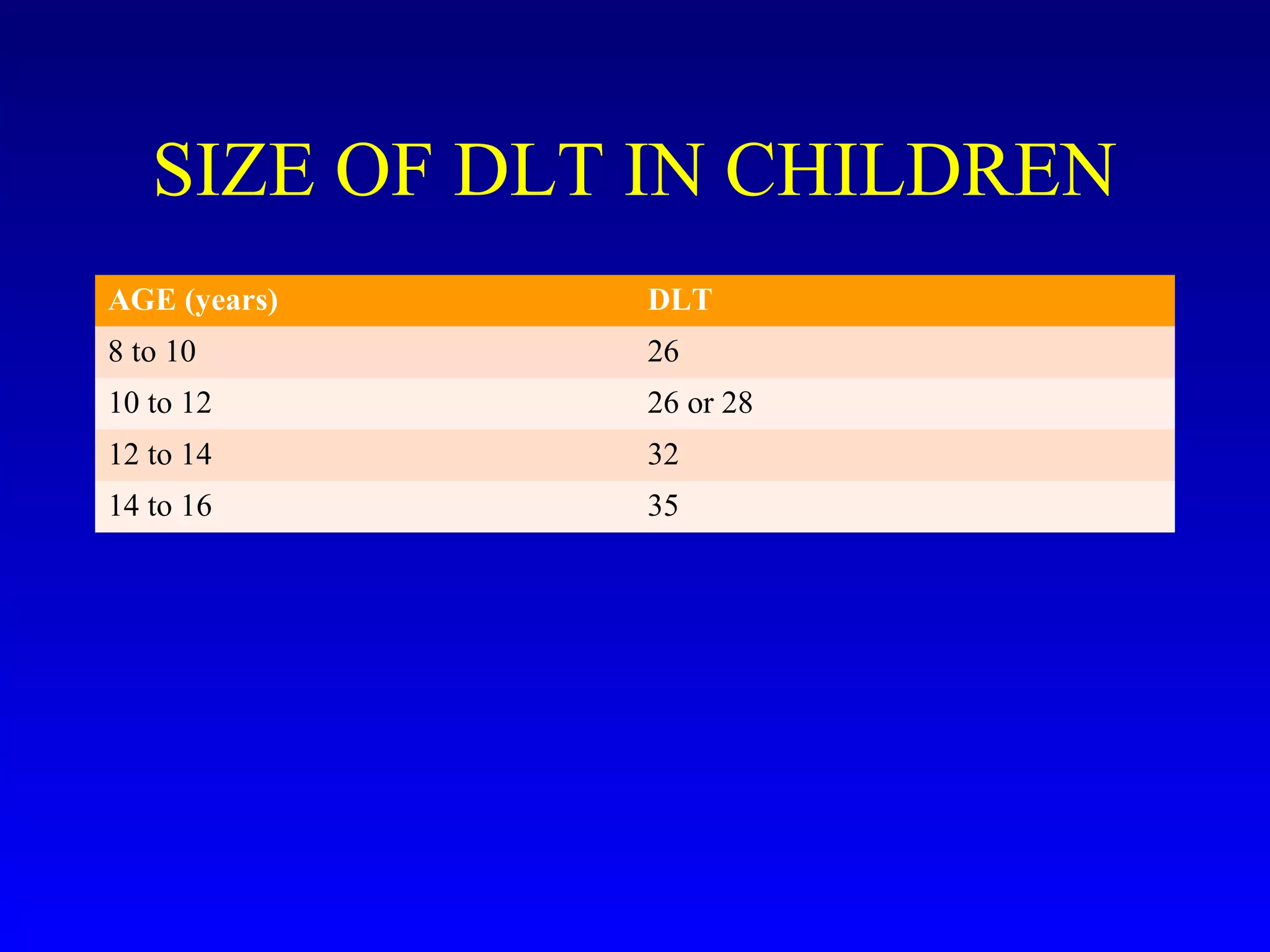
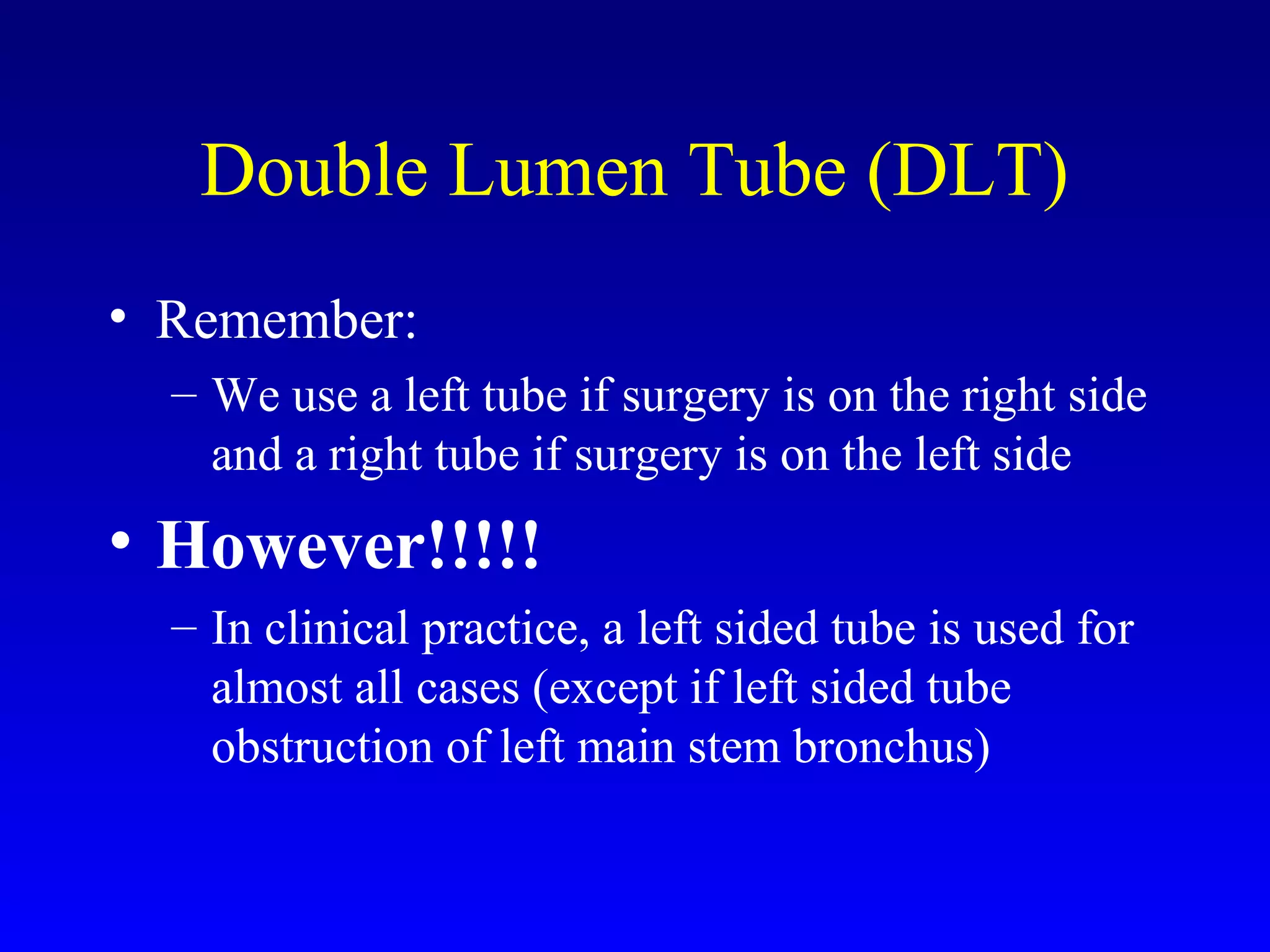
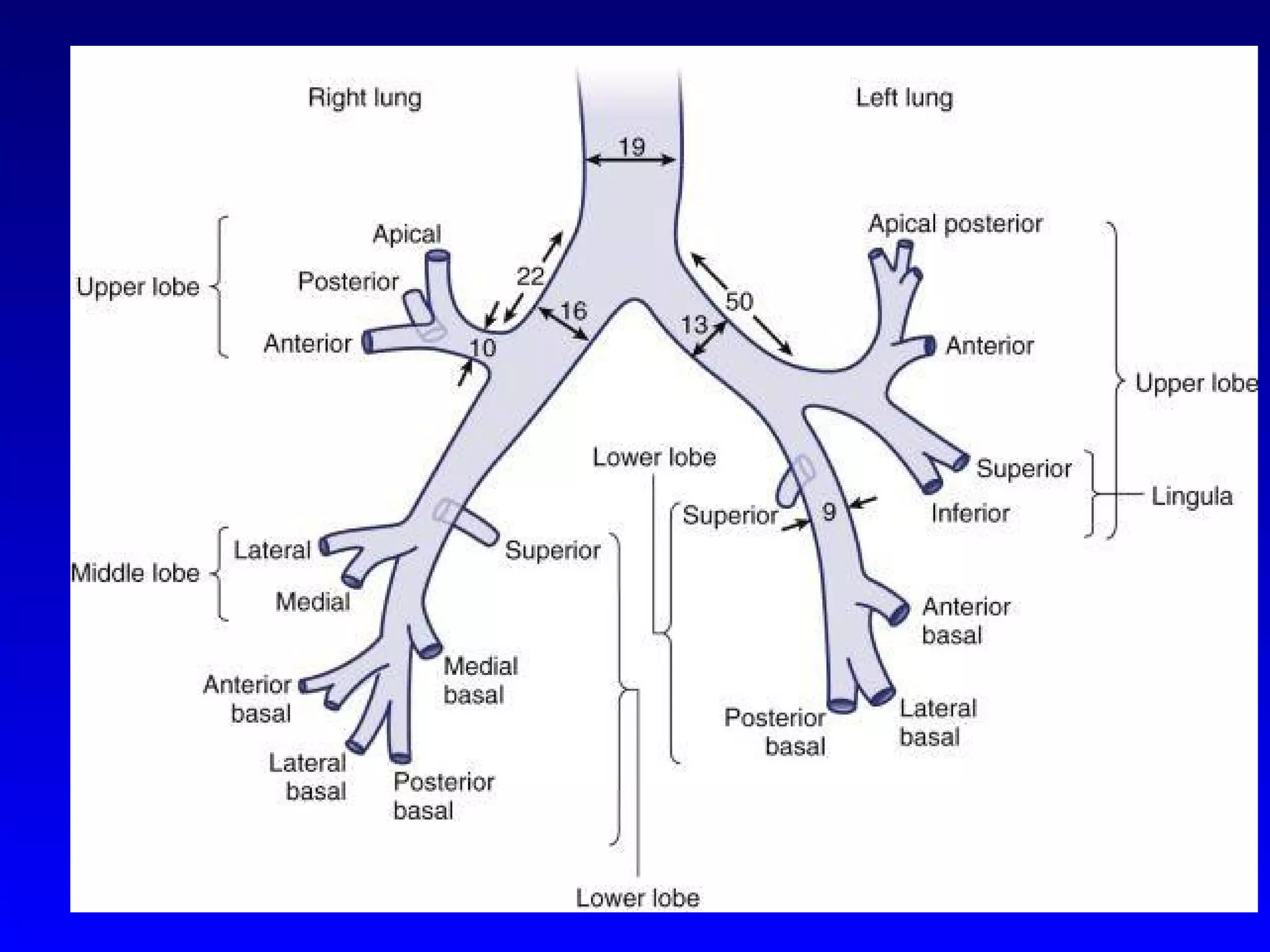
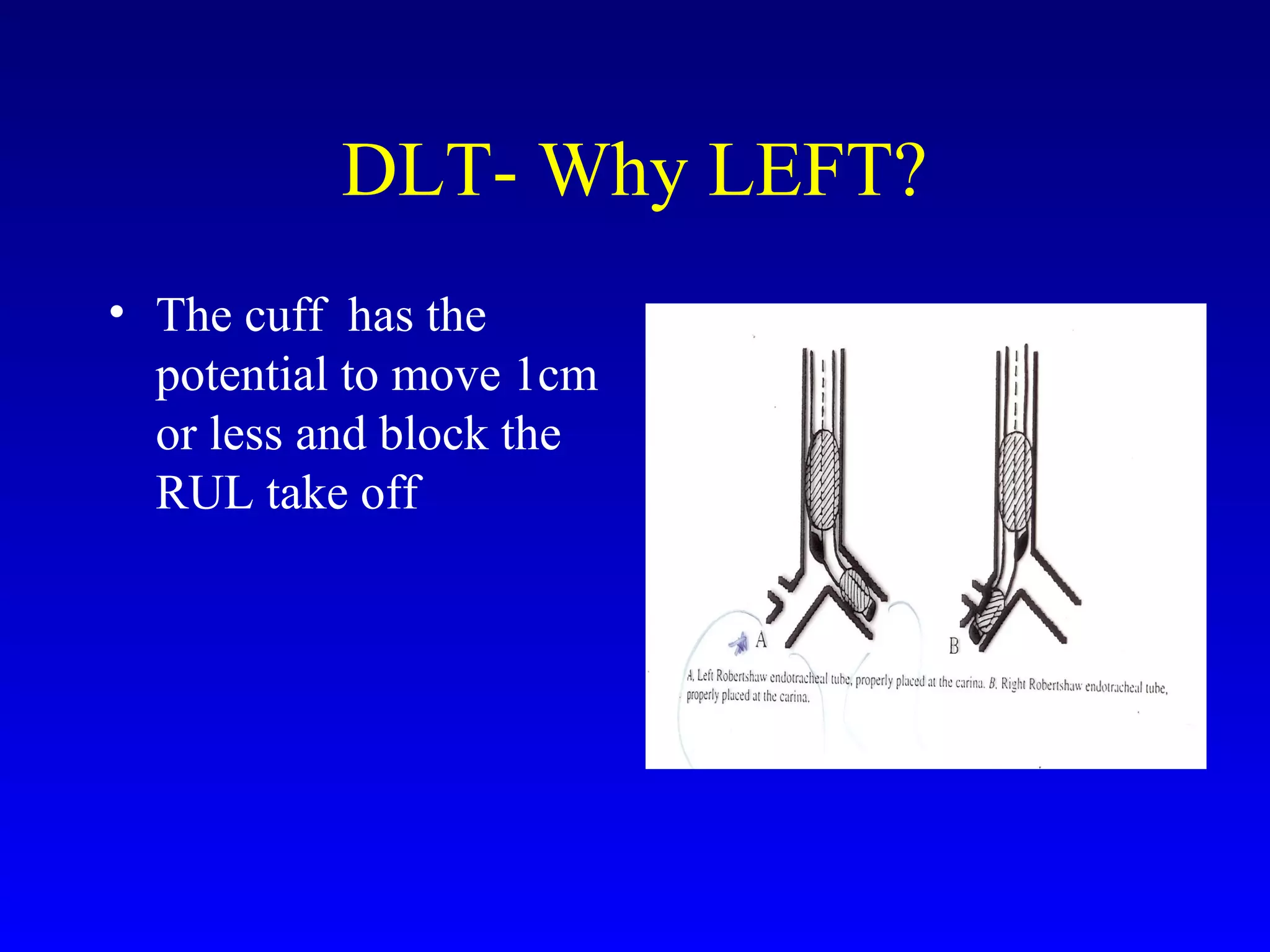
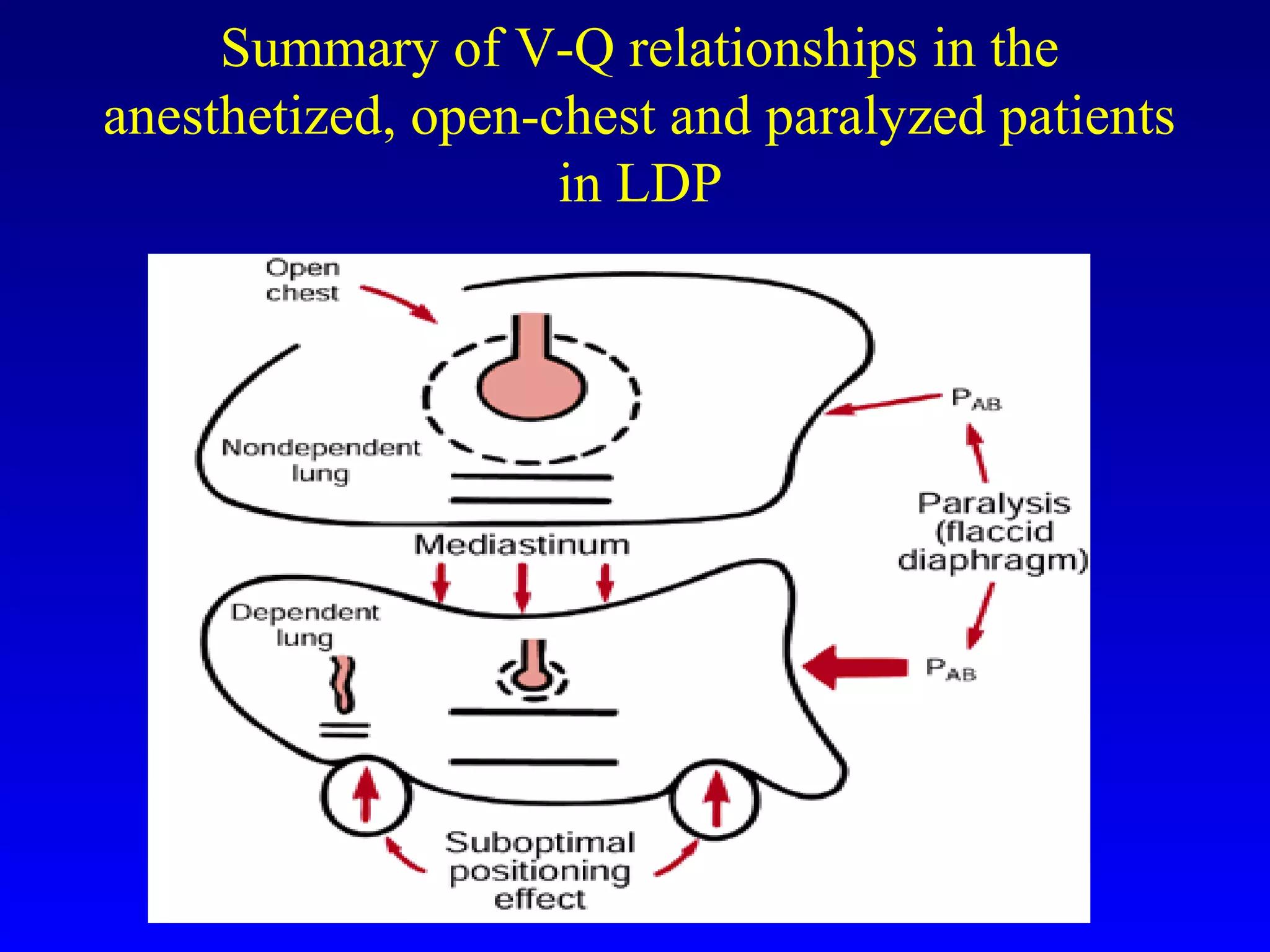
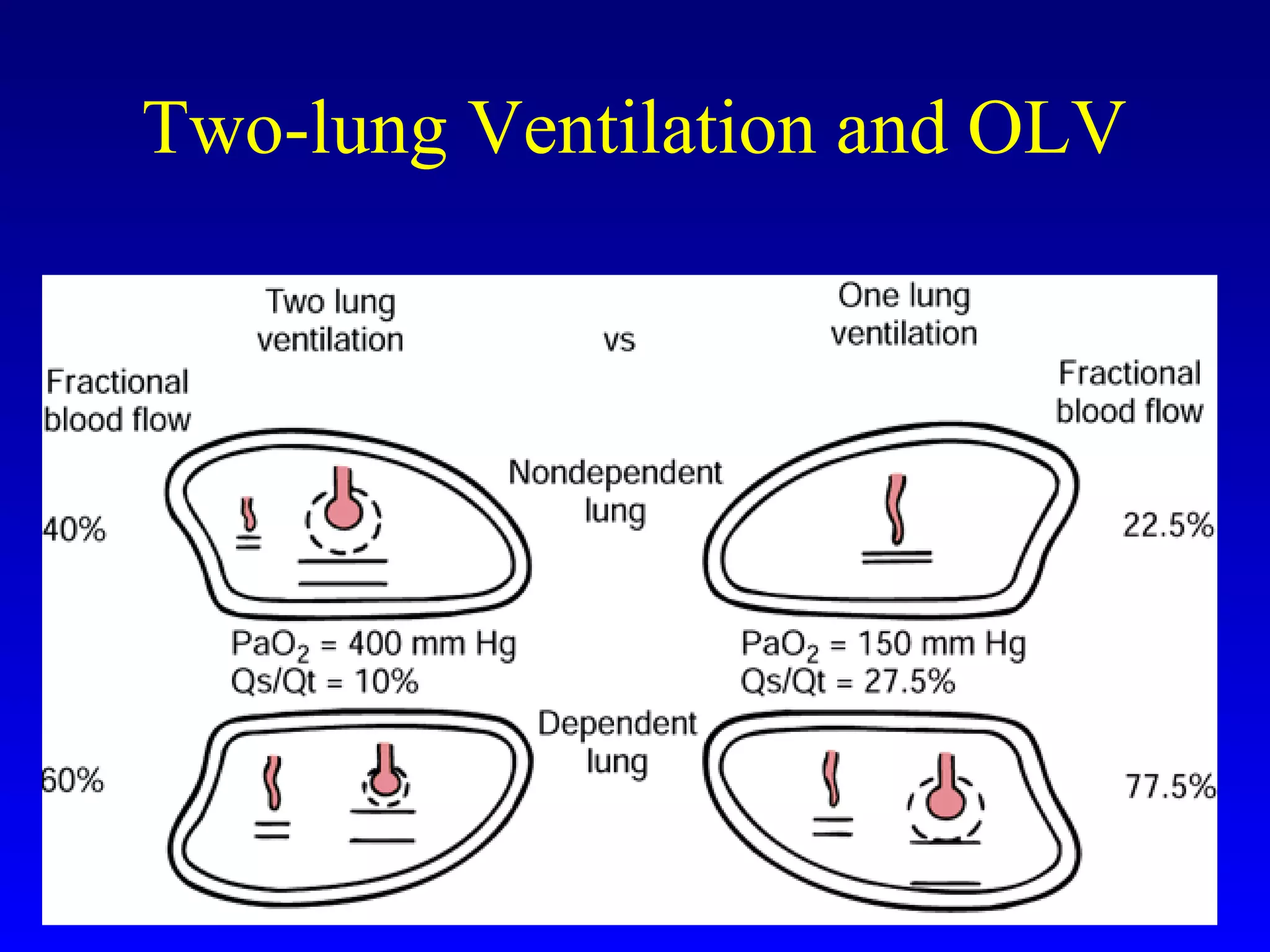
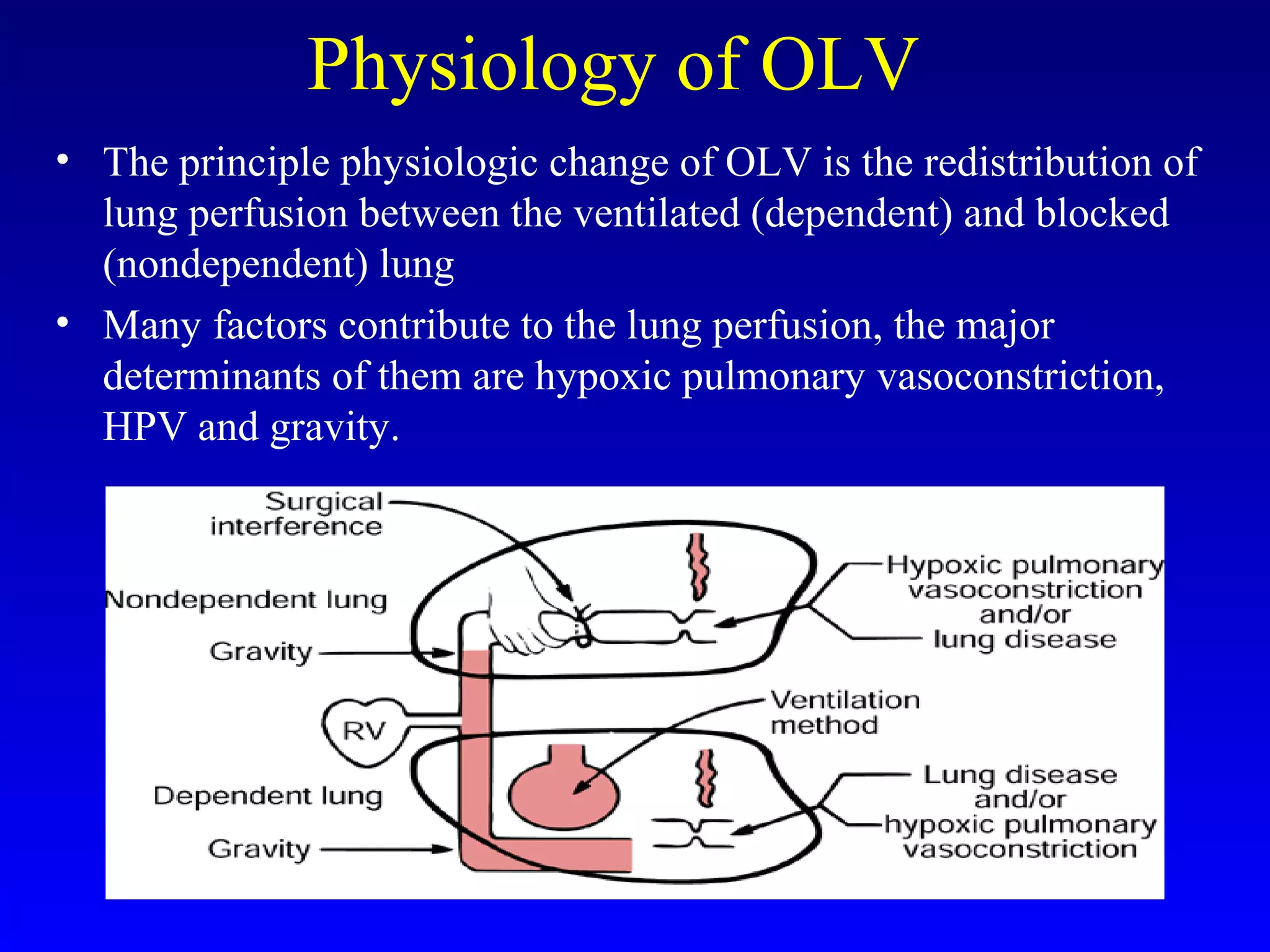
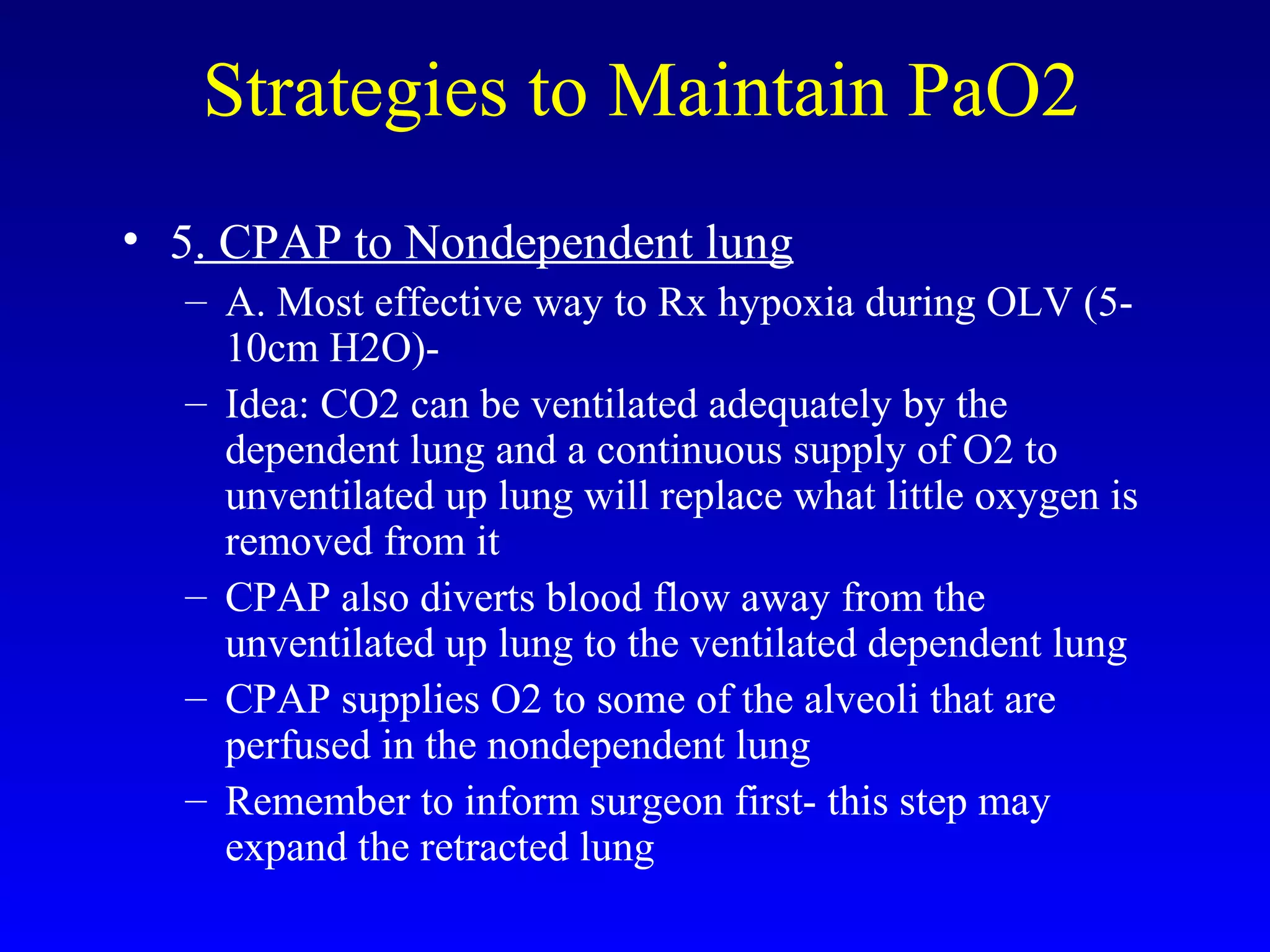
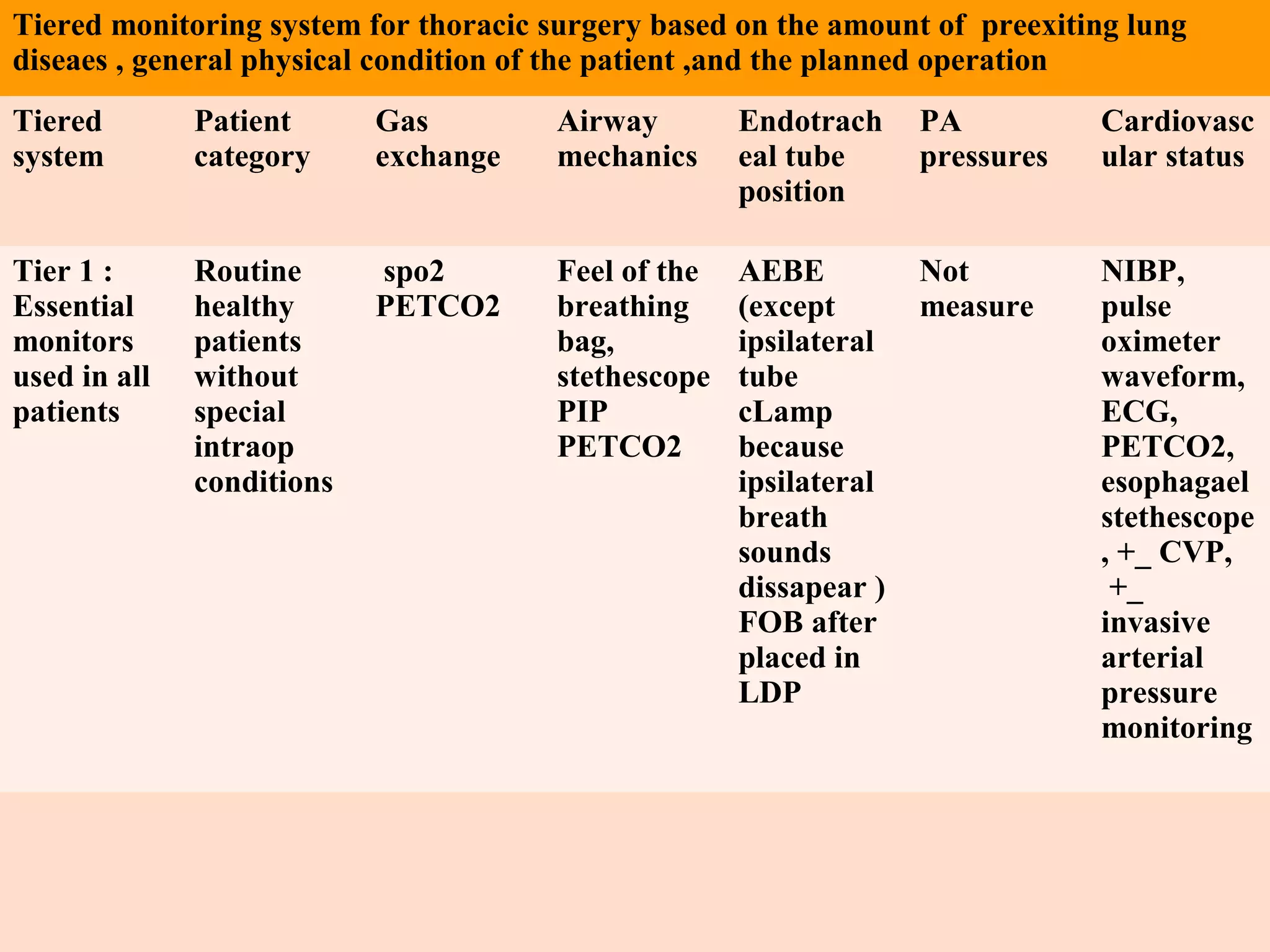
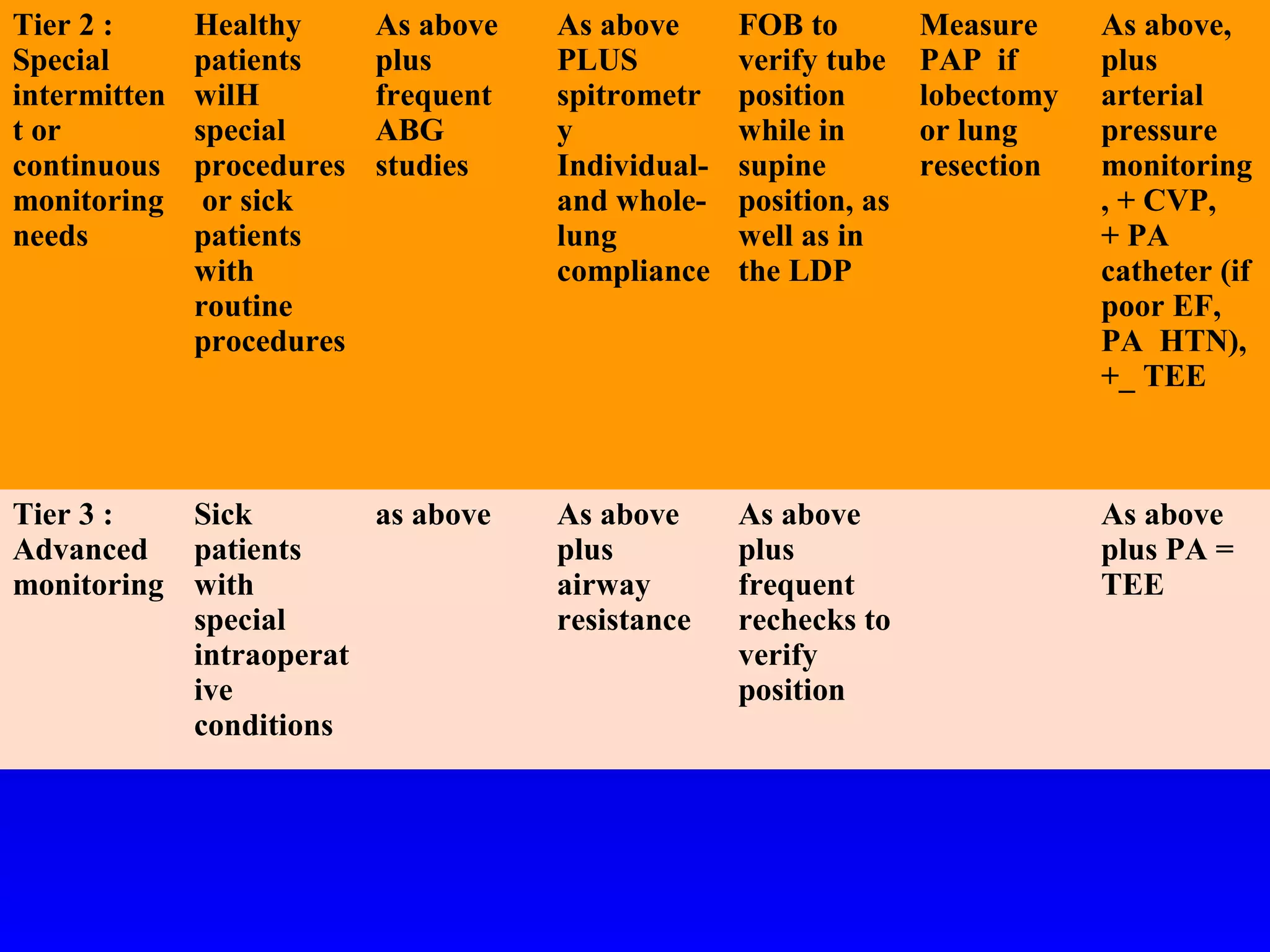
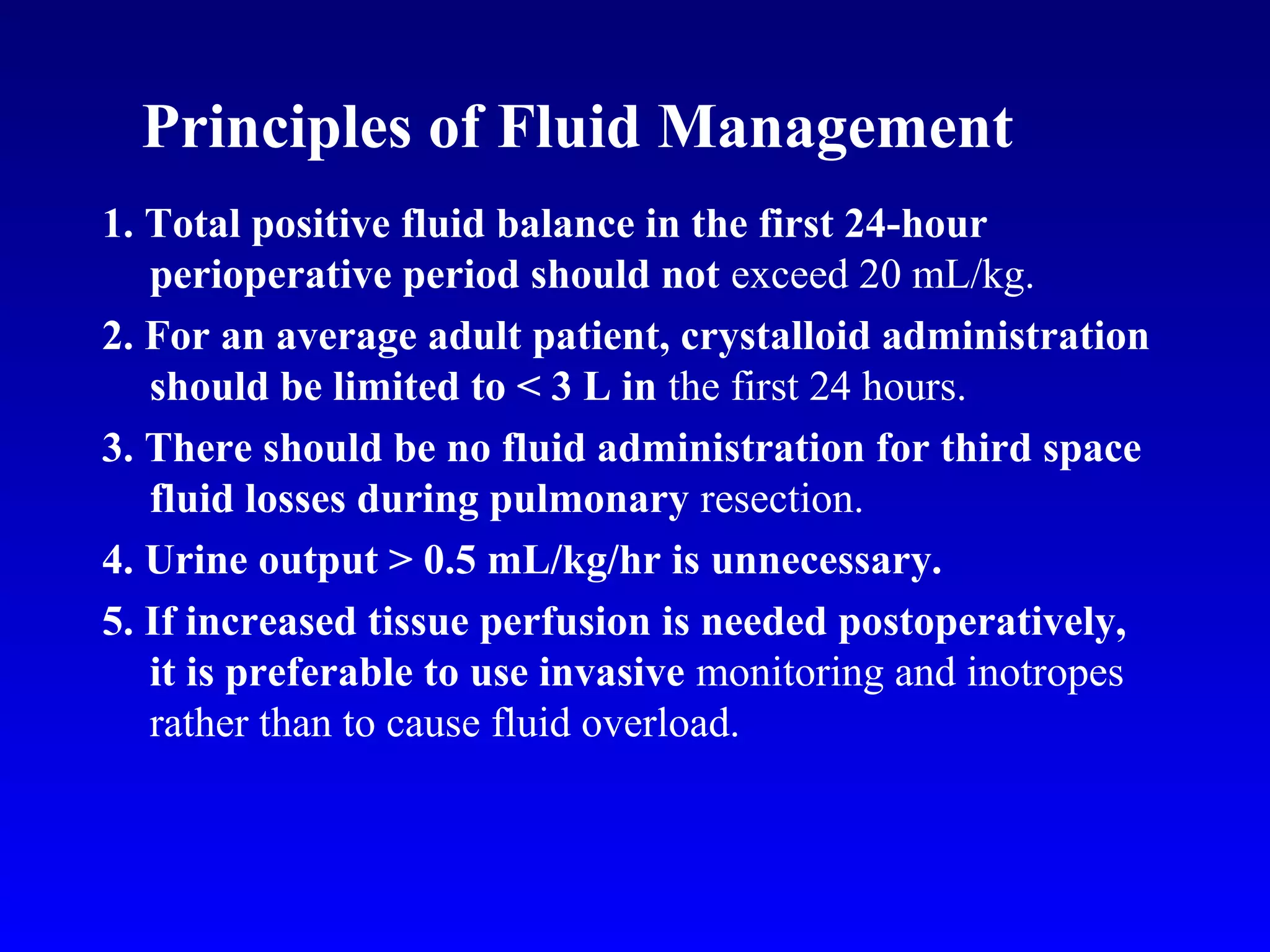
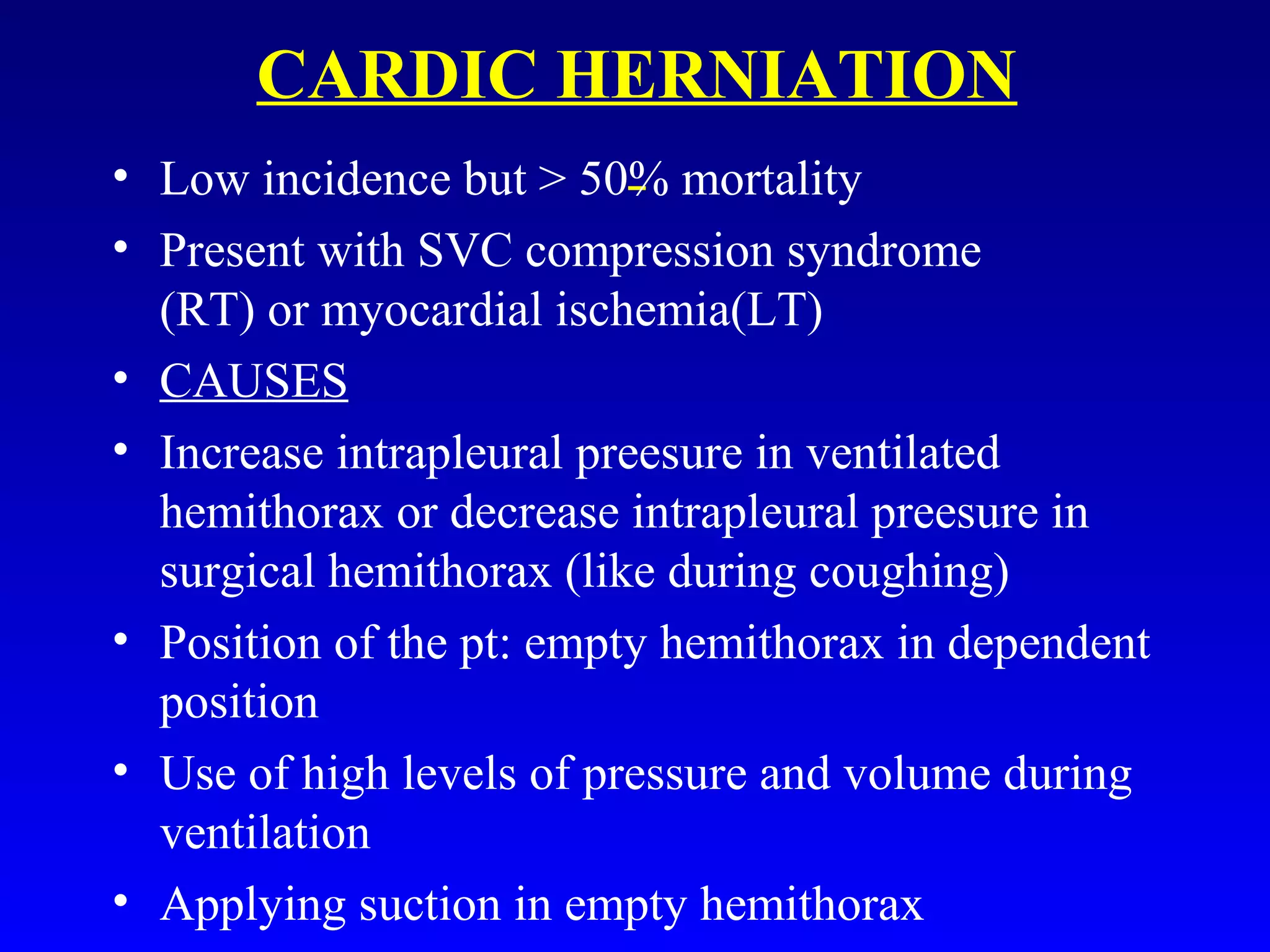
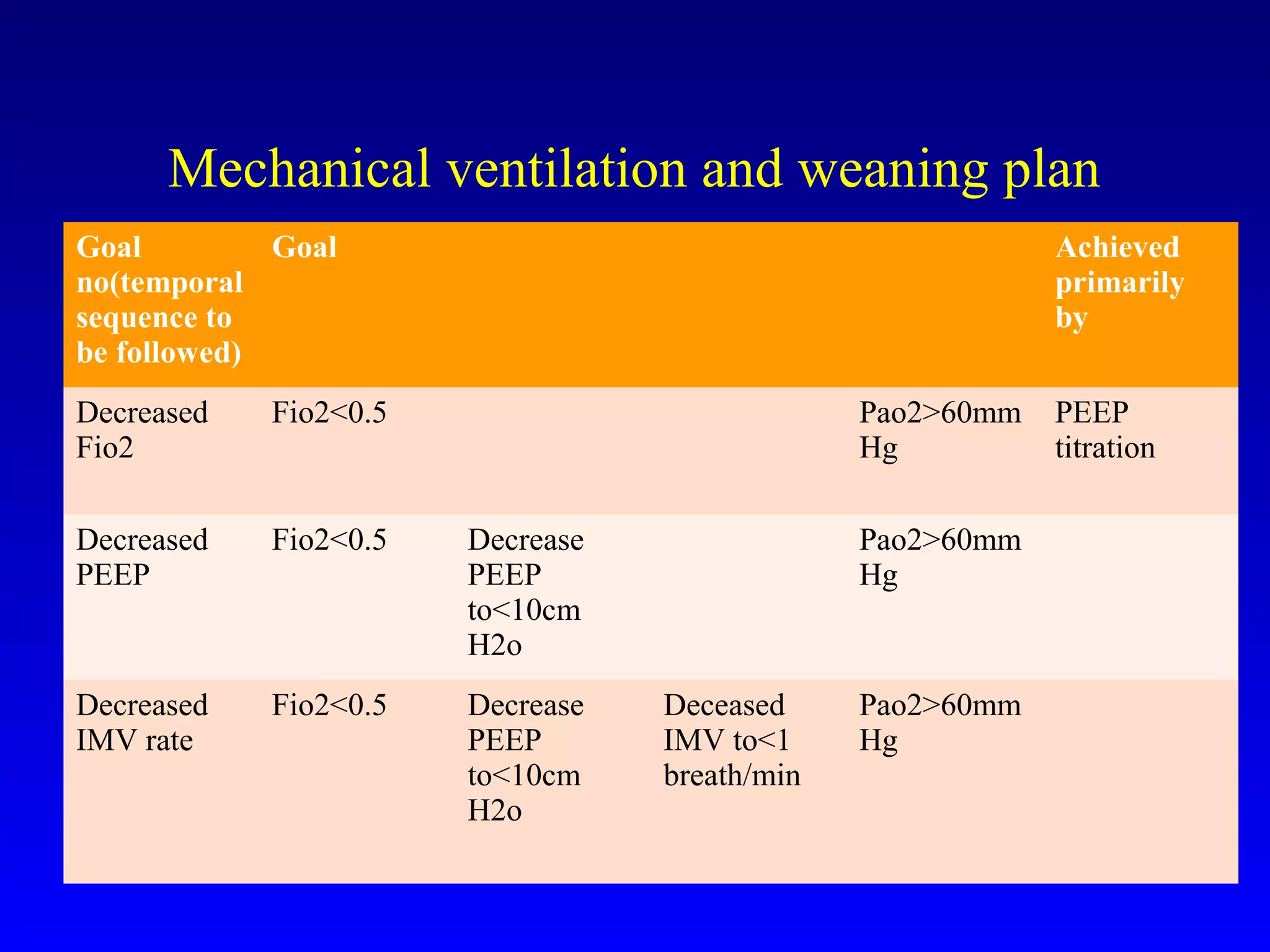
3) Anesthetic management focuses on techniques for one-lung ventilation using devices like double-lumen endotracheal tubes, as well as strategies for ventilation, induction, and analgesia tailored to patient comorbidities.