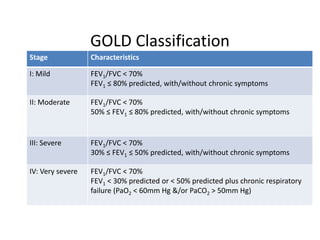
This document discusses COPD pathophysiology and anesthetic management. It begins by defining COPD and describing its risk factors such as smoking. It then explains the disease pathogenesis involving inflammation, tissue destruction, and proteinase-antiproteinase imbalance. Pathology of the large and small airways and parenchyma are described. Outcomes like airflow obstruction and hyperinflation are discussed. The GOLD classification stages COPD severity. Treatment includes smoking cessation, bronchodilators, pulmonary rehabilitation and managing exacerbations. The document outlines pre-operative assessment including history, exams, investigations like CXR and PFTs. It provides guidance on pre-operative preparation and intraoperative and postoperative risk reduction strategies like regional anesthesia