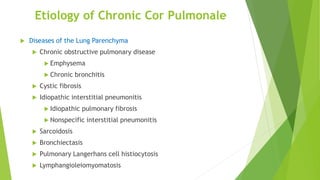
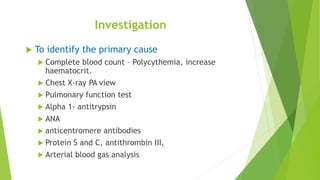
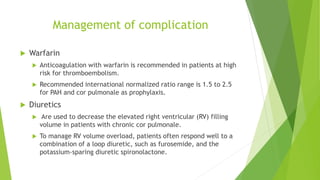
Cor pulmonale is right ventricular heart failure caused by lung disease that leads to pulmonary hypertension. The most common cause is chronic obstructive pulmonary disease. It can be acute or chronic. Treatment focuses on managing the underlying lung condition, treating pulmonary hypertension with medications, diuretics for volume overload, anticoagulation for those at high risk of clots, and oxygen therapy. Prognosis depends on the specific lung disease, with cor pulmonale due to conditions like COPD generally having a poorer long term outlook.