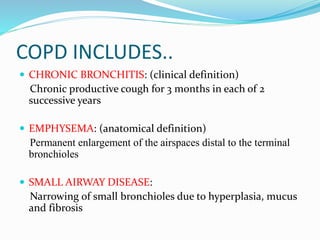
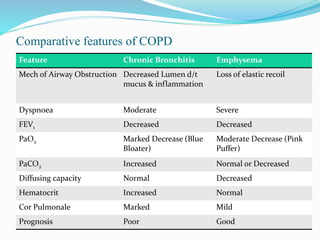
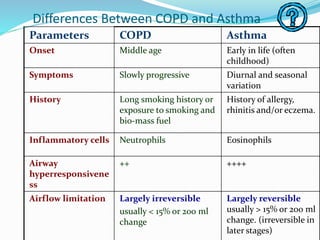
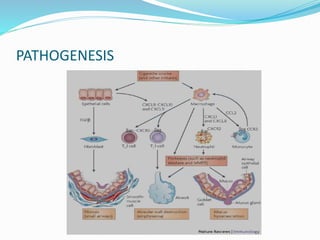
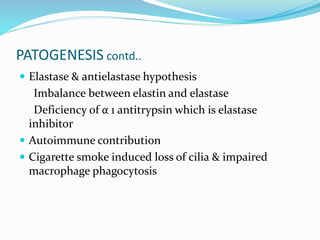
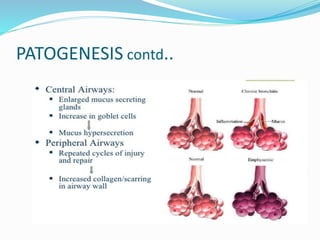
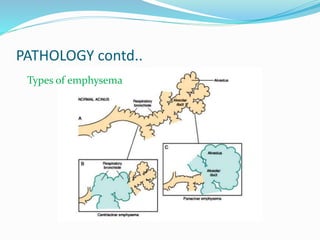
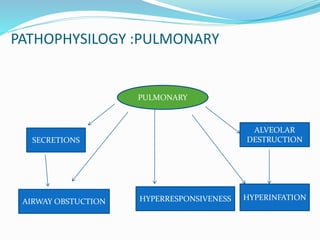
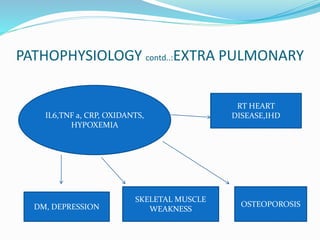
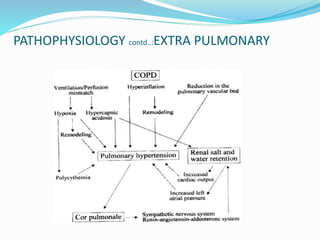
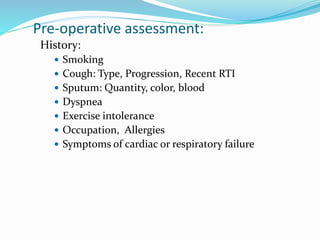
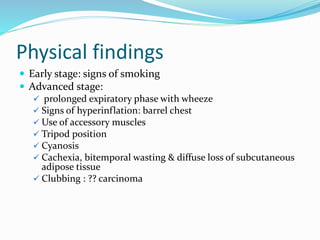
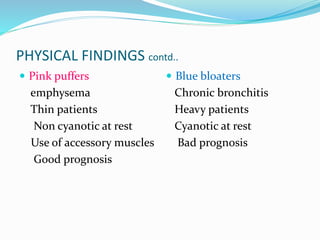
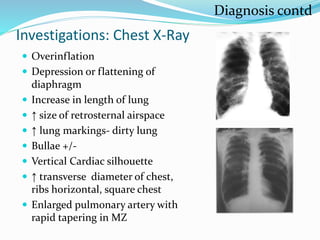
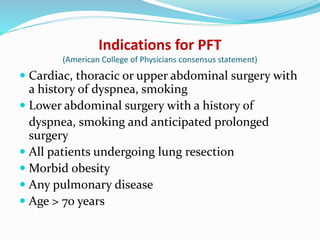
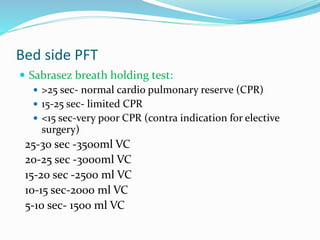
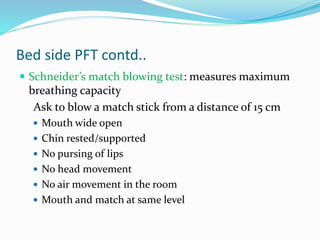
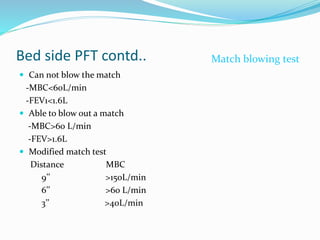
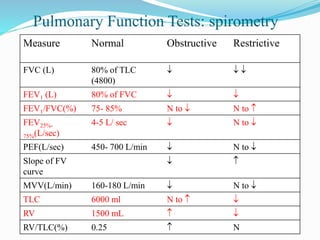
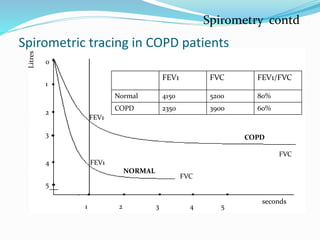
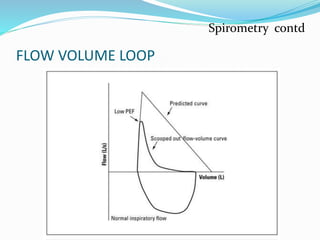
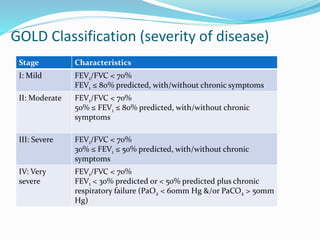
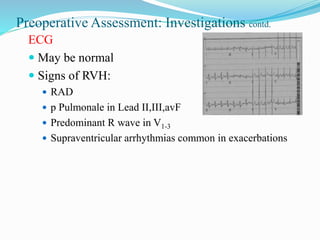
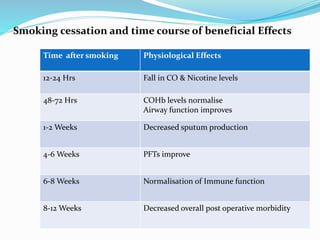
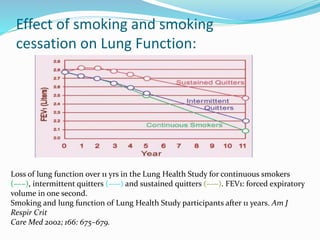
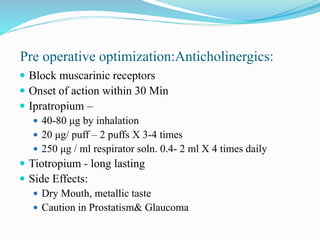
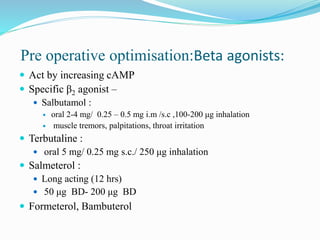
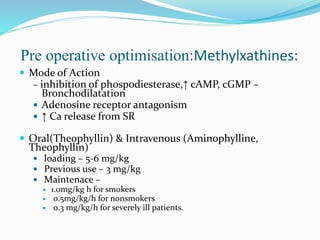
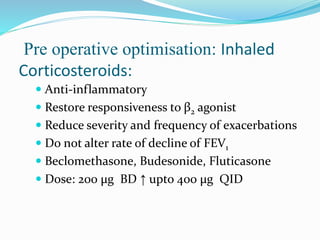
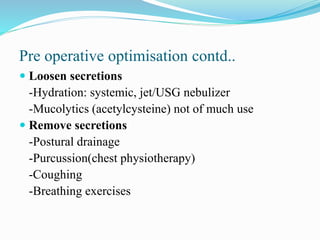
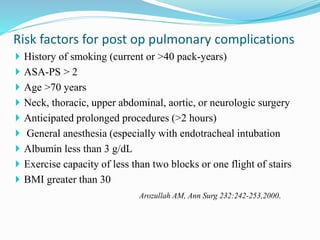
This document provides information on chronic obstructive pulmonary disease (COPD) including its definition, pathophysiology, diagnosis, and pre-operative optimization. It defines COPD as a common lung disease characterized by persistent airflow limitation associated with an enhanced inflammatory response in the airways. The document discusses the types and features of COPD including chronic bronchitis and emphysema. It covers the risk factors, pathogenesis, pathology, and pathophysiology of COPD. Details are provided on pre-operative patient assessment including history, physical exam, investigations like chest x-ray, spirometry, ABG and optimization measures such as smoking cessation and bronchodilation therapy.