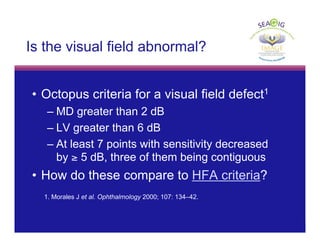
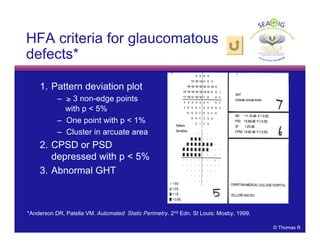
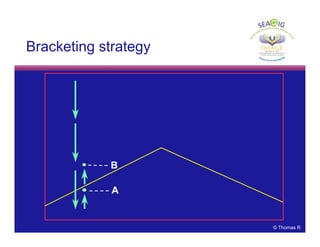
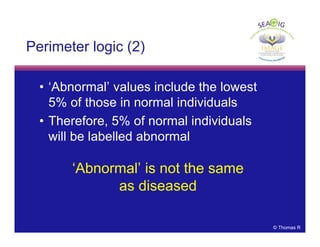
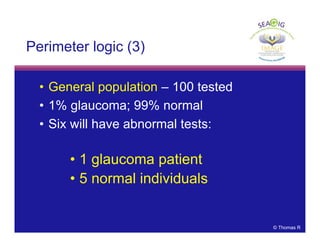
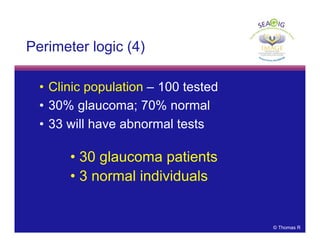
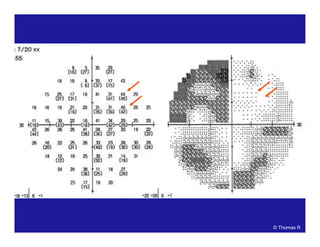
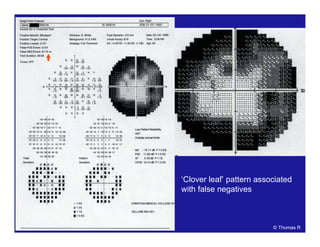
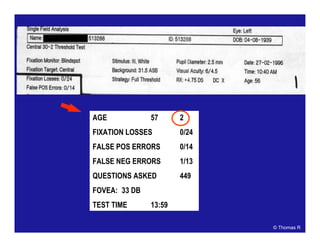
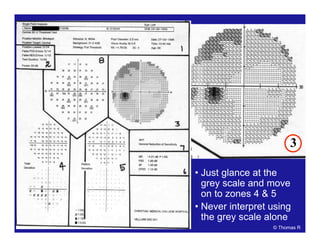
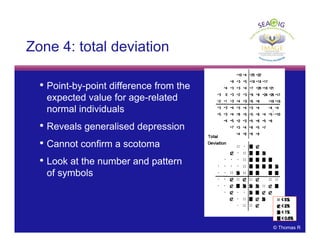
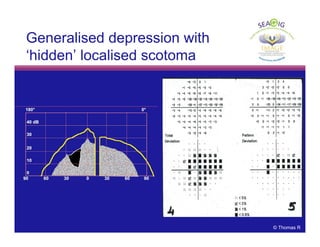
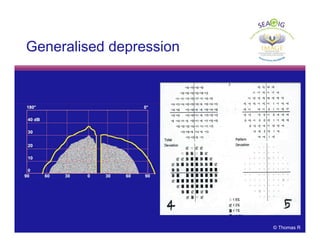
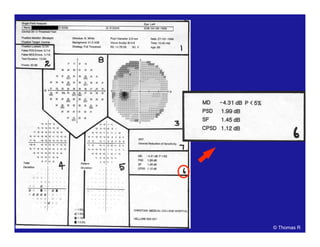
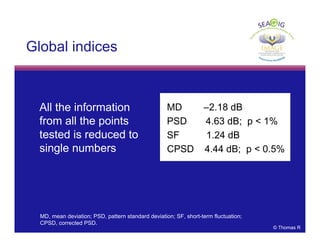
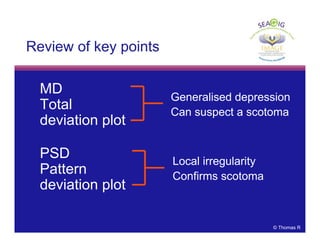
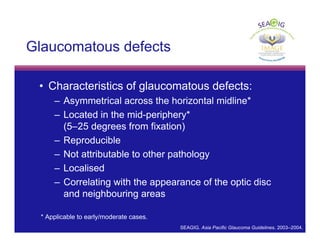
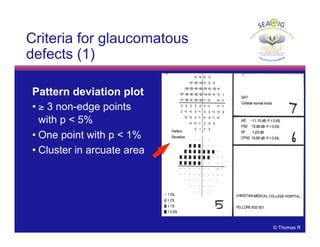
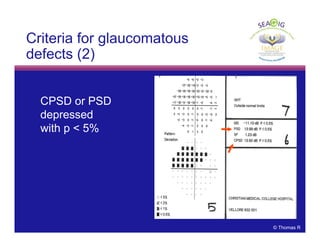
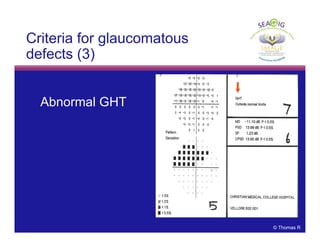
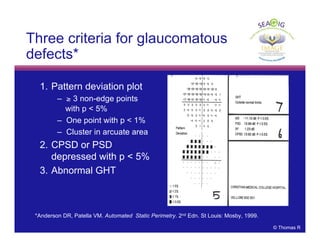
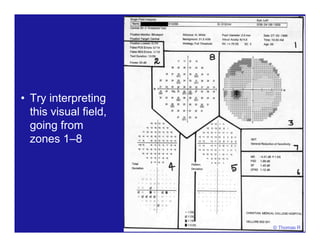
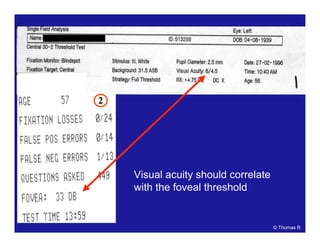
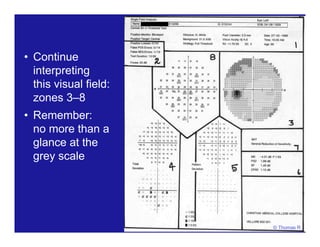
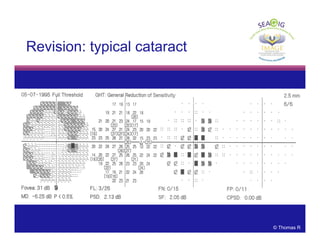
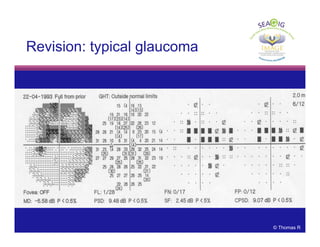
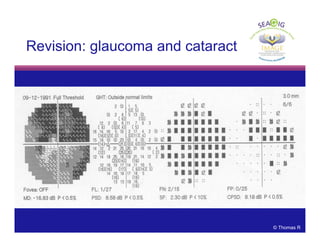
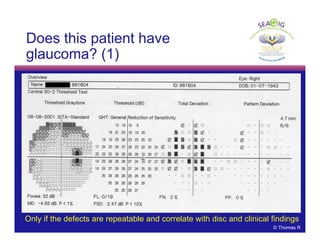
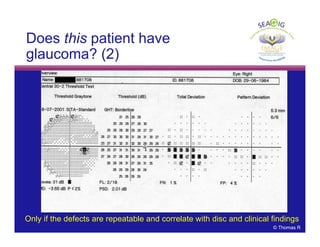
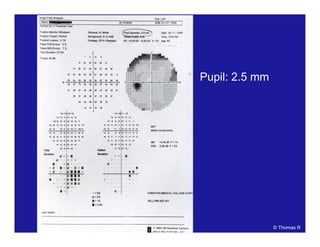
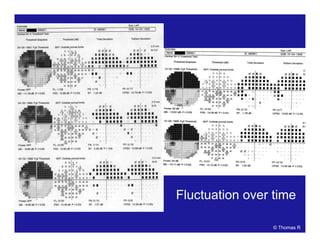
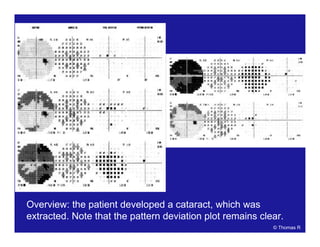
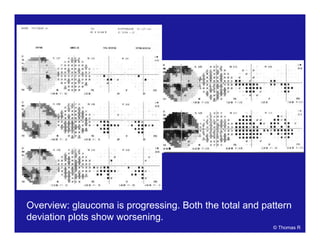
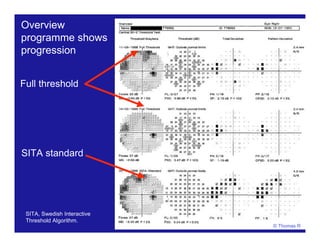
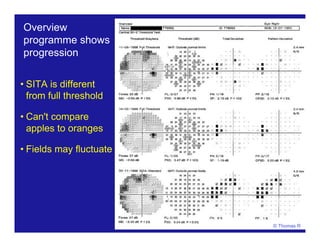
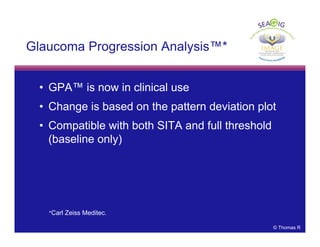
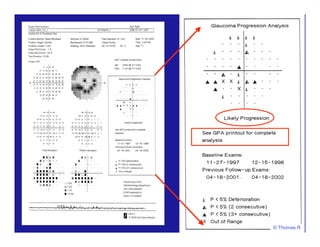
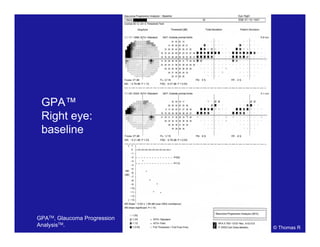
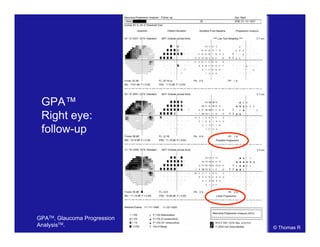
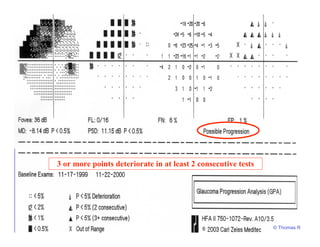
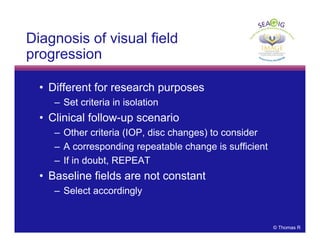
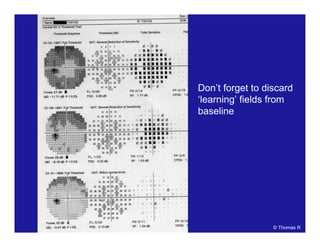
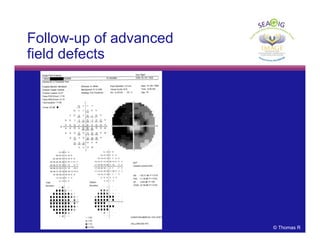
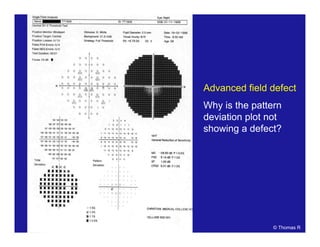
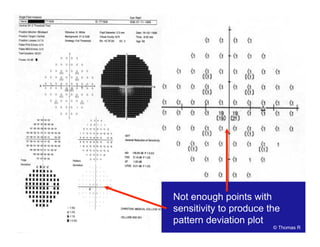
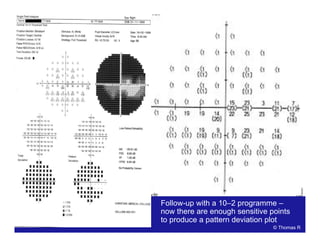
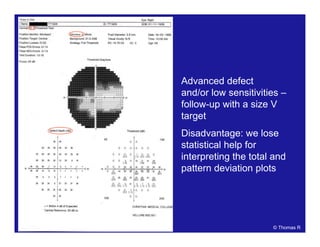
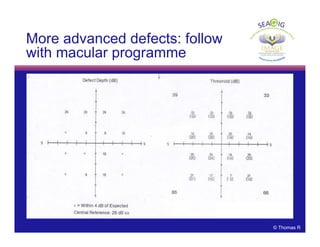
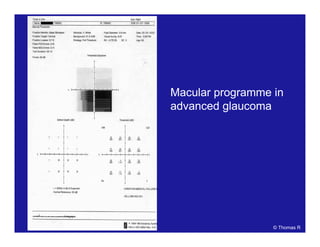
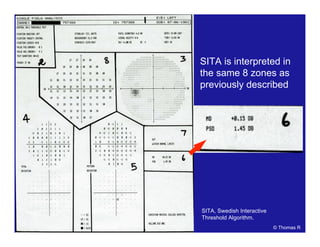
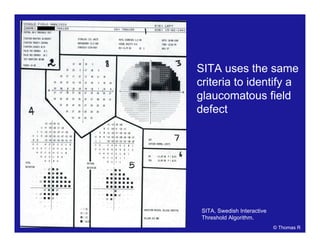
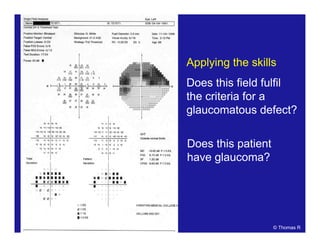
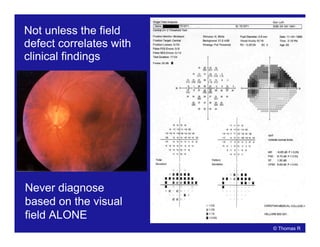
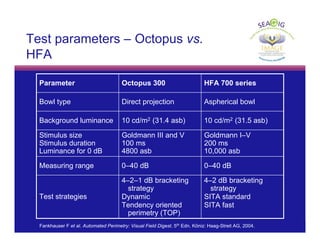
This document discusses automated perimetry and the interpretation of visual field tests. It covers perimeter logic and identifying field defects, criteria for glaucomatous defects, and detecting glaucomatous progression. Key points include interpreting visual fields systematically using total and pattern deviation plots in 8 zones, criteria for identifying glaucomatous defects including abnormalities in the pattern deviation plot, global indices, and techniques for detecting progression such as the overview program and Glaucoma Progression Analysis. Interpretation requires correlating results with clinical findings and considering factors like learning effects and fluctuation.
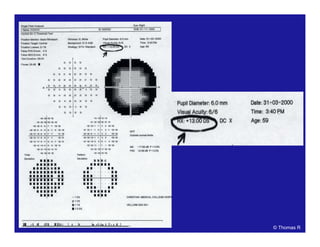
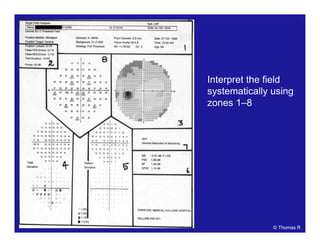
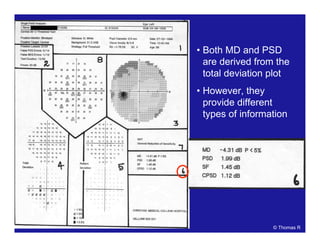


![[[Credit line to be added]]
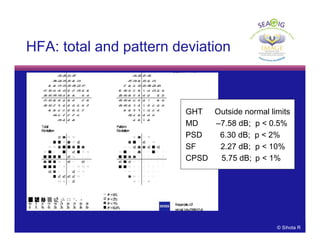
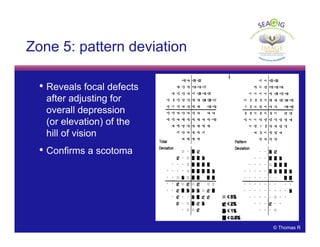
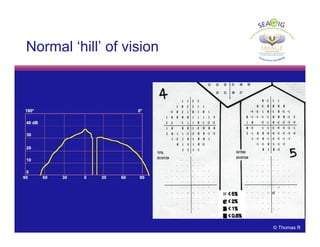
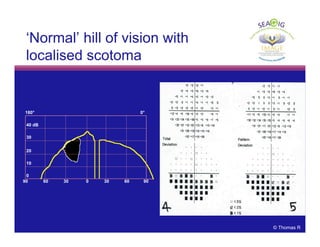
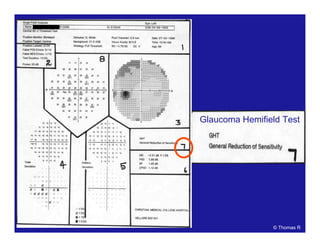
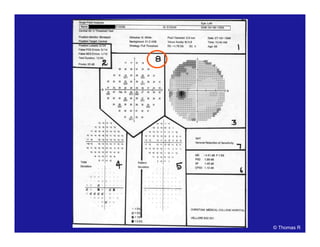
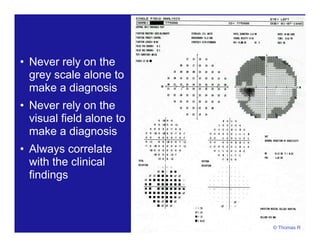
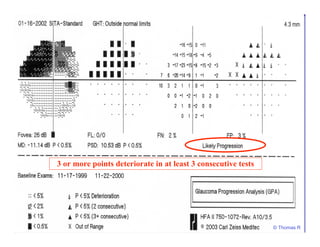
Probability
plots
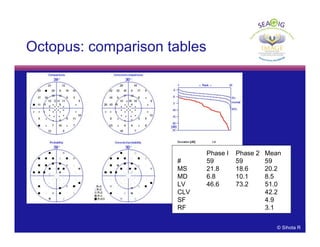
Comparison
tables
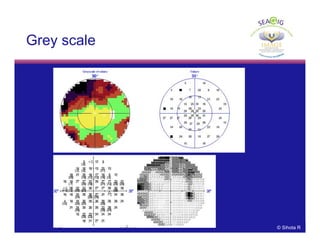
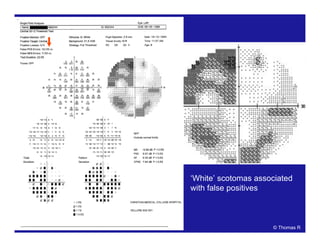
Grey scale
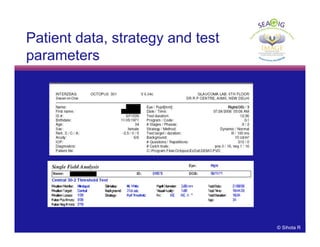
Patient data
and refraction
Strategy and
test parameters
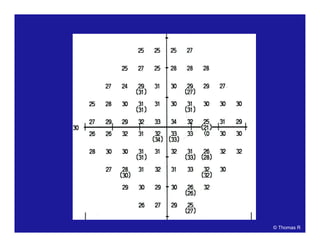
Actual values
Bebie (defect)
curve
Deviation
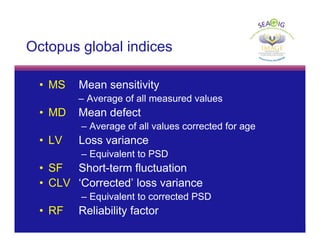
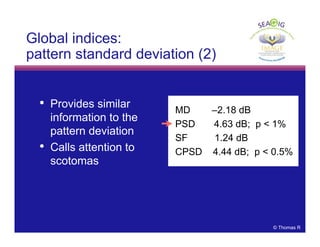
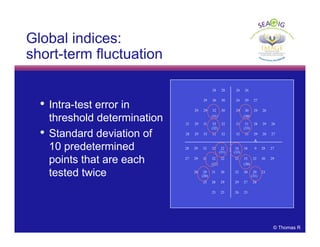
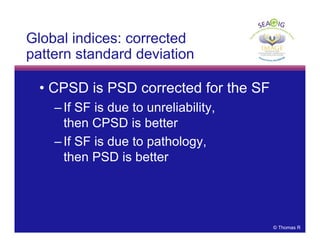
Global indices
RP: permission
requested](https://image.slidesharecdn.com/autoperinm-130613000312-phpapp02/85/Auto-perimetry-108-320.jpg)